INTRODUCTION
The health effects of cigarette smoking have been well documented. Smoking harms almost every organ of the human body and causes a range of diseases, including cardiovascular disease, respiratory disease, cancers, some mental health issues and other health problems1-3. However, the relationship between having health problems (including comorbidity) and interest in quitting and cessation outcomes is complex and under-studied in nationally representative surveys.
An early descriptive study observed that hospitalization in the preceding two years was associated with a 30–40% greater likelihood of smoking cessation4. Diagnosis of smoking related cancers such as lung and head/neck cancers has been found to be associated with high increased desire for smoking cessation5,6. Persons diagnosed with hypertension and chronic heart disease, chronic obstructive pulmonary disease (COPD) and diabetes have also been found to have a greater desire to quit smoking, although this has not always translated into higher rates of smoking abstinence6-12. It should be noted that most of the available research reported above had small samples and was conducted mostly in the context of hospitalization or outpatient care. Nationally representative population data have been little employed to examine the relationship between physical illness and desire for smoking cessation.
Much is known about the relationship between mental health conditions and smoking/cessation. People with mental health problems are more likely to smoke, and to smoke more heavily, than the general population2,13,14. The smoking prevalence among people with clinical depression is approximately twice that of the general population15,16. Comorbid disorders are associated with higher proportions of heavy smoking2. Smoking rates have declined in the general population over the last few decades but not among people with indicators of longstanding mental disorders or recent psychoactive medication usage17. A recent study in the UK found equivocal evidence, but the gap in smoking between the general population and those with mental disorders is not closing18. Depression, especially severe depression, seems to make it difficult for smokers to quit even though they are aware of the long-term harms of smoking2,19,20. In England, although people with mental health problems are more likely to be advised to quit by general practitioners; when the number of consultations is taken into account, they are actually less likely to be so advised21. Cessation rates remain consistently lower for depressed smokers than for smokers in the general population, highlighting a need to better understand their associations and identify more effective intervention strategies22. Identified mechanisms that underline persistent smoking among depressive smokers include low positive affect, high negative affect and cognitive impairment22.
The present study aimed to examine whether having health conditions or concerns related to smoking are associated with quitting activities, including intention/self-efficacy to quit, making quit attempts, and use of stop-smoking medications in reported quit attempts, and whether the associations differ by country. We expect to find greater quitting activity among those with illnesses strongly causally linked to smoking, and based on past work, more so among those with mental health problems. But we are less certain as to what to expect for other conditions with more complex relationships, such as chronic pain and obesity, where smoking may be used as part of self-management. We also expect higher levels of use of stop-smoking medications, as those with health conditions are likely to be in contact with health professionals who should be recommending them.
METHODS
Data source and participants
The data came from Wave 1 of the International Tobacco Control Four Country Smoking and Vaping Survey (ITC 4CV1) conducted in Australia, Canada, England and the United States from July to November 2016. The valid main sample (n=12294) consisted of the following respondent groups: 1) adult smokers and quitters who responded to previous ITC 4C Surveys23, and were successfully re-contacted online; 2) current smokers and past smokers who had quit smoking in the past two years, and were newly recruited in 2016 through online probability-based consumer panels; and 3) newly recruited current electronic cigarette (e-cigarette) users. The sample was designed to be representative of tobacco and e-cigarette users in each country. Because the current study is mainly concerned about the associations between a range of reported health problems and combustible tobacco use/quitting among cigarette smokers and recent quitters who stopped smoking in the past two years, a total of 74 cases of non-smokers (never smokers) and 382 cases who were re-contacted from a previous ITC 4C Survey but who had been abstinent for more than two years were excluded from the analysis. Hence, our analytic sample consisted of a total of 11838 respondents (Australia: n=1490; Canada: n=3576; England: n=4220; and US: n=2552), among whom 47.1% were exclusive cigarette smokers, 6.4% exclusive e-cigarette users, 27.4% concurrent users, and 19.1% were recent cigarette quitters. Table 1 presents sample size and characteristics by country. A more detailed description of sampling methods and original sample size for each country can be found elsewhere23-25.
Table 1
Weighted sample characteristics, by country
| Characteristics | Canada n=3576 % | US n=2552 % | England n=4220 % | Australia n=1490 % | Total n=11838a % | p-value for χ2 |
|---|---|---|---|---|---|---|
| Gender (Female) | 41.5 | 45.5 | 46.2 | 44.5 | 44.4 | <0.05 |
| Age (years) | <0.001 | |||||
| 18–24 | 13.2 | 10.7 | 15.9 | 12.5 | 13.6 | |
| 25–39 | 29.9 | 31.8 | 35.4 | 37.3 | 33.3 | |
| 40–54 | 30.9 | 29.1 | 25.3 | 27.5 | 28.1 | |
| ≥55 | 26.1 | 28.3 | 23.2 | 22.7 | 25.1 | |
| Ethnicity | <0.001 | |||||
| White | 84.7 | 78.2 | 94.1 | 89.6 | 87.2 | |
| Non-White (minority group) | 15.3 | 21.8 | 5.9 | 10.4 | 12.8 | |
| Educationb | <0.001 | |||||
| Low | 27.2 | 50.9 | 17.7 | 38.5 | 30.4 | |
| Moderate | 45.7 | 33.8 | 63.6 | 36.5 | 48.4 | |
| High | 26.5 | 15.3 | 15.9 | 23.9 | 20.1 | |
| Incomeb | <0.001 | |||||
| Low | 34.1 | 36.8 | 20.4 | 30.5 | 29.3 | |
| Moderate | 24.1 | 31.7 | 43.9 | 23.9 | 32.7 | |
| High | 34.8 | 30.6 | 26.6 | 38.1 | 31.3 | |
| No information | 7.1 | 1.0 | 9.2 | 7.5 | 6.6 | |
| Cigarette smoking status | <0.001 | |||||
| Recent quitter | 26.1 | 21.8 | 27.2 | 26.2 | 25.6 | |
| Non-daily smoker | 21.9 | 14.6 | 18.2 | 7.0 | 17.1 | |
| Daily smoker | 52.1 | 63.9 | 54.7 | 66.8 | 57.4 | |
| Respondent type | <0.001 | |||||
| Exclusive smoker | 41.4 | 55.9 | 42.1 | 58.8 | 47.1 | |
| Concurrent user | 32.5 | 22.3 | 30.8 | 15.1 | 27.4 | |
| Exclusive vaper | 6.0 | 4.5 | 9.5 | 2.3 | 6.4 | |
| Former smoker | 20.1 | 17.3 | 17.6 | 23.9 | 19.1 |
Measures
Self-reported health problems
All respondents were asked whether they were currently being treated for or had been diagnosed (current diagnosis) with three types of health problems related to cigarette smoking: 1) those where there are strong causal links (heart disease; cancer, excluding non-melanoma skin cancer; and chronic lung disease such as chronic bronchitis and emphysema); 2) those that are mental health related (i.e. depression, anxiety, alcohol problems); and 3) those with more complex associations (severe obesity, chronic pain, and diabetes). Their answers were coded as ‘yes, selected’ vs ‘not selected/don't know’. In England, respondents were asked about lung cancer and other cancers separately, and instead of chronic lung disease, they were asked about four specific conditions: asthma, emphysema, chronic bronchitis and tuberculosis, with respondents reporting any specific condition classified as having the general condition. We also conducted supplementary analyses on a composite of having any of the three mental health conditions and any of the three conditions most commonly caused by smoking (cancer, heart disease, and lung disease).
In addition, participants were asked: ‘To what extent, if at all, has smoking cigarettes damaged your health?’, and (for current smokers only) ‘How worried are you, if at all, that smoking cigarettes will damage your health in the future?’. The response options for both were: ‘not at all’, ‘just a little’, ‘a fair amount/moderately’, ‘a great deal’, and ‘don't know’. The responses were recoded into ‘yes, at least moderately’ vs all lesser responses and don't know.
Quit-related measures
Current smokers were asked: ‘Are you planning to quit smoking?’. Response options were ‘within the next month’, ‘within the next 6 months’, ‘sometime in the future, beyond 6 months’, and ‘not planning to quit’. The first two categories were recoded as ‘within the next 6 months’, and the remaining as ‘no current plans’ (which also included ‘don't know’). Self-efficacy to quit was assessed by asking: ‘If you decided to give up smoking completely in the next 6 months, how sure are you that you would succeed?’ (‘not at all sure/slightly/don't know’ vs ‘moderately/very/extremely sure’). Quit attempts were assessed by asking current smokers who reported ever making quit attempts: ‘How many times, if any, have you tried to quit in the past 12 months?’ (‘no attempt’ including ‘never tried’ vs ‘1 or more attempts’). Those who reported having made at least 1 quit attempt in the last 12 months were also asked about their use of stop-smoking medications (coded as ‘any type of nicotine replacement therapy (NRT), varenicline or bupropion’ vs ‘no medication)’ in their last quit attempt.
Other covariates
Demographics measures included age (18–24, 25–39, 40–54, ≥55 years), sex (male, female), and ethnicity (White/English-speaking in Australia vs non-White/non-English-speaking/identified-minority-group). Due to the differences in economic development and educational systems across countries, only relative levels of income and education were used. ‘Low’ level of education referred to those who completed high school or less in Canada, the US and Australia, and secondary/vocational or less in England; ‘moderate’ meant community college/trade/technical-school/some university (no degree) in Canada and the US, college/university (no degree) in England, or technical/trade/some university (no degree) in Australia; and ‘high’ referred to those who completed university or postgraduate studies in all countries. Household annual income was also grouped into ‘low’ (<US$30000 in the US, <AU$45000 in Australia, <CA$45000 in Canada, <£15000 in England), ‘moderate’ (US$30000–$59999, AU$45000–$74999, CA$45000–$74999, £15000–£39999), and ‘high’ categories (≥US$60000, ≥AU$75000, ≥CA$75000, ≥£40000).
Cigarettes smoking status was also asked and recoded into three categories: daily smokers, non-daily smokers and recent quitters. As in previous research26, depending on respondents’ cigarette and e-cigarette use, we re-categorized respondents into the following four types: cigarette-only smokers, concurrent users, e-cigarette-only users, and ex-smokers (Table 1).
Data analysis
The analysis was weighted and the stratified sampling design was accounted for. The prevalence/proportions of key measures are reported. For categorical variables, chi-squared tests were performed to check for equality of percentages in subgroups/countries. To compare self-reported health conditions across countries and quitting activities (e.g. whether having plans to quit) for each health condition separately, we employed logistic regression, controlling for sociodemographics. We also tested for interactions by health condition with country, but only retained interaction effects in the models when they were significant. In these cases, follow-up analyses stratified by country were then conducted, and relevant results on country differences are reported. In all analyses, a p-value <0.05 was considered statistically significant. All analyses were conducted using Stata Version 14.1.
The survey protocols and all materials, including the survey questionnaires, were cleared for ethics by Institutional Review Board, Medical University of South Carolina (ORE No. 20803); Research Ethics Office, King’s College London, UK (ORE No. 20803 and RESCM-17/18-2240); Office of Research Ethics, University of Waterloo, Canada (ORE No. 20803 and ORE No. 21609); and Human Research Ethics, Cancer Council Victoria, Australia (ORE No. 21609 and HREC 1603).
RESULTS
Sample characteristics
Table 1 presents weighted sample characteristics in the four countries. Overall, respondents were more likely to be male, White, and aged ≥40 years. In all four countries, the biggest respondent type was exclusive cigarette smokers, followed by concurrent users of cigarettes and e-cigarettes, ranging from 15% in Australia to over 30% in both Canada and England. About a quarter of respondents were recent quitters. Among the continuing smokers, 36.6% planned to quit smoking within the next 6 months; 48.7% had at least moderate self-efficacy to quit; 48.8% reported at least 1 quit attempt in the past 12 months; and of those daily smokers who made quit attempts in the last year (n=4534), 40.5% reported using some form of smoking cessation medication (any of NRT, varenicline or bupropion) in their last quit attempts.
Overall, more people reported mental health conditions (e.g. about 21% reported depression) than physical conditions (e.g. 11.1% reported chronic pain), and the most severe physical conditions were generally reported at the lowest levels (e.g. only 3.9% reported heart disease). There were marked differences in rates of reporting conditions by country with respondents from England least likely to report these health conditions (Supplementary file, Table 1).
Quitting activities and use of cessation medications among those with or without health problems
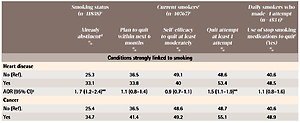
Table 2 shows the relationships between health conditions and quitting measures. The four measures of interest in quitting (being abstinent, planning to quit within the next 6 months, past attempts, and use of stop-smoking medications) were generally higher in those with the conditions, and self-efficacy generally lower, although not always significantly. These are noted in Table 2 but details are provided below. There were, by country, relatively few statistically significant health-condition interaction effects.
Table 2
Association between self-reported health problems and quitting activities (in all 4 countriesa)
| Smoking status (n=11838)c | Current smokerse (n=10767)c | Daily smokers who made >1 attempt (n=4534)c | |||
|---|---|---|---|---|---|
| Already abstinentd % | Plan to quit within next 6 months % | Self-efficacy to quit at least moderately % | Quit attempt at least 1 attempt % | Use of stop smoking medications to quitf (Yes) % | |
| Conditions strongly linked to smoking | |||||
| Heart disease | |||||
| No (Ref). | 25.3 | 36.5 | 49.1 | 48.6 | 40.6 |
| Yes | 33.1 | 33.8 | 40 | 53.4 | 48.5 |
| AOR (95% CI)g | 1. 7 (1.2–2.4)** | 1.1 (0.8–1.4) | 0.9 (0.7–1.1) | 1.5 (1.1–1.9)** | 1.1 (0.8–1.6) |
| Cancer | |||||
| No (Ref). | 25.4 | 36.5 | 48.6 | 48.7 | 40.6 |
| Yes | 34.7 | 41.4 | 49.2 | 55.1 | 48.9 |
| AOR (95% CI) | 1.8 (1.2–2.8)** | 1. 5 (1.1–2.1)* | 1.3 (0.9–1.8) | 1. 5 (1.1–2.1)* | 1. 1 (0.6–2.1) |
| Chronic lung disease | |||||
| No (Ref). | 25.6 | 36.4 | 49.2 | 48.3 | 40.2 |
| Yes | 25.6 | 39.6 | 39.2 | 55.8 | 47.8 |
| AOR (95% CI) | 1. 1 (0.8–1.5) | 1.3 (1.1–1.6)* | 0.8 (0.6–0.9)* | 1.5 (1.2–1.8)*** | 1.3 (0.9–1.8) |
| Mental health conditions | |||||
| Depression | |||||
| No (Ref.) | 25.3 | 35.8 | 49.8 | 47.4 | 39.2 |
| Yes | 26.3 | 39.5 | 44.9 | 54.2 | 46.6 |
| AOR (95% CI) | 1.1 (0.9–1.3) | 1.2 (1.1–1.3)* | 0.8 (0.7–0.9)** | 1.3 (1.1–1.4)** | 1.4 (1.1–1.7)** |
| Anxiety | |||||
| No (Ref). | 25 | 35.9 | 49.6 | 47.6 | 39.4 |
| Yes | 27.9 | 39.1 | 45.1 | 53.8 | 46.5 |
| AOR (95% CI) | 1.5 (1.1–2.1)*b | 1.1 (0.8–1.3)b | 0.8 (0.7–0.9)** | 1.2 (1.1–1.4)** | 1.5 (1.2–1.9)** |
| Country interactions | Significant (see text) | Significant (see text) | NS | NS | NS |
| Alcohol problems | |||||
| No (Ref). | 25.8 | 36.2 | 48.9 | 48.7 | 40.5 |
| Yes | 11.5 | 44.2 | 44.6 | 52.7 | 55.2 |
| AOR (95% CI) | 0.4 (0.2–0.9)** | 0.8 (0.5–1.4)b | 0.8 (0.6–1.1) | 0.8 (0.5–1.3)b | 2.0 (0.9–4.5)b |
| Country interactions | NS | Significant (see text) | NS | Significant (see text) | Significant (see text) |
| Conditions with complex relationships with smoking | |||||
| Diabetes | |||||
| No (Ref). | 25.4 | 36.8 | 49.1 | 48.5 | 40.1 |
| Yes | 26.8 | 32.6 | 45.5 | 53.1 | 49.4 |
| AOR (95% CI) | 1. 2 (0.9–1.6) | 1.0 (0.8–1.2) | 1.1 (0.9–1.3) | 1.4 (1.1–1.7)** | 1.2 (0.9–1.7) |
| Severe obesity | |||||
| No (Ref). | 25.2 | 36.2 | 48.9 | 48.4 | 40.5 |
| Yes | 35.7 | 44.5 | 43.2 | 61.3 | 51.2 |
| AOR (95% CI) | 1. 7 (1.2–2.6)** | 1.4 (1.1–1.9)* | 0.8 (0.6–1.1) | 1.6 (1.2–2.3)** | 1.4 (0.9–2.3) |
| Chronic pain | |||||
| No (Ref). | 25.5 | 36.6 | 49.7 | 48.3 | 39.4 |
| Yes | 25.2 | 36.6 | 41.2 | 52.8 | 51.2 |
| AOR (95% CI) | 1.1 (0.9–1.4) | 1.1 (0.9–1.3) | 0.7 (0.5–0.9)*b | 1.3 (1.1–1.5)** | 1.4 (1.1–1.8)* |
| Country interactions | NS | NS | Significant (see text) | NS | NS |
| General concerns about harms of smoking | |||||
| Smoking has damaged health | |||||
| No (Ref). | 23.9 | 33.7 | 52.2 | 44.9 | 38.7 |
| Yes | 27.2 | 42.8 | 44.7 | 57.7 | 43.5 |
| AOR (95% CI) | 1.3 (1.1–1.6)** | 1.7 (1.4–2.4)***b | 0.8 (0.7–0.9)*** | 1.8 (1.6–2.0)*** | 1.1 (0.9–1.4) |
| Country interactions | NS | Significant (see text) | NS | NS | NS |
| Smoking will damage health | |||||
| No (Ref). | N/A | 23.5 | 51.7 | 36.7 | 42.5 |
| Yes | 45.6 | 46.5 | 57.1 | 45.1 | |
| AOR (95% CI) | 2.7 (2.4–3.1)*** | 0.9 (0.8–1.2)b | 2.3 (2.1–2.6)*** | 1.1 (0.9–1.3) | |
| Country interactions | NS | Significant (see text) | NS | NS | |
a Wherever significant health condition by country interaction effects were identified, follow-up analyses stratified by country were conducted, and relevant results were reported in the main text.
b With significant health condition by country interaction effects. NS: No significant health condition by country interaction effects.
d The analysis was weighted and the stratified sampling design was accounted for, and this applies to all outcomes.
For diseases strongly linked to smoking, there were more reported quit attempts with all three conditions; increased likelihood of being abstinent for cancer and heart disease (but not chronic lung conditions), and more future plans for cancer and chronic lung conditions (but not heart disease, Table 2). No associations were found between these health conditions and use of cessation medications on the last quit attempt. When combined as a group, we found that having ‘any’ of these three smoking-caused conditions was associated with having made quit attempts (55.6% vs 47.6%; adjusted odds ratio, AOR=1.6; 95% CI: 1.4–1.9; p<0.001), and more planning to quit (39.1% vs 36.1%; AOR=1.4; 95% CI: 1.2–1.6; p<0.001).
Turning to mental health conditions, having alcohol problems was associated with being less likely to be a recent ex-smoker, and among smokers there were significant by country interaction effects for all quitting measures except self-efficacy. For example, in England, those with alcohol problems were more likely to plan to quit (56.5% vs 35.1%; AOR=2.4; 95% CI: 1.4–4.0; p<0.01) and have made attempts (57.2% vs 45.3%; AOR=1.8; 95% CI: 1.1–3.1; p<0.05), with no evidence of effects in the other three countries for these two quitting measures. In Australia, those daily smokers with alcohol problems were more likely to use medications to quit (72.3% vs 40.3%; AOR=3.1; 95% CI: 1.1–8.3; p<0.05), but in the other three countries there were no significant differences in use of medications between those with and without alcohol problems.
Those with depression or anxiety were more likely to report quit attempts, to use quit medications, and had lower self-efficacy than those without the corresponding condition. However, they varied on plans to quit where those with depression were generally more likely to plan future attempts, but for anxiety this was only true in the US (40.3% vs 29.1%; AOR=1.5; 95% CI: 1.1–2.0; p<0.01), whereas in Australia, those with anxiety were less likely to plan to quit (34.3% vs 42.1%; AOR=0.6; 95% CI: 0.4–0.9; p<0.05). Those with anxiety were also more likely to be abstinent, but the by-country interaction suggests this was mainly so in Canada (32.5% vs 24.5%; AOR=1.5; 95% CI: 1.1–2.0; p<0.05).
In the supplementary analyses, we found those having ‘any’ of these three mental health conditions were more likely to have made attempts (52.7% vs 46.8%; AOR=1.2; 95% CI: 1.1–1.4: p<0.01), use cessation medications (46.6% vs 38.6%; AOR=1.5; 95% CI: 1.2–1.8; p<0.001), plan future attempts (39.6% vs 35.3%; AOR=1.2; 95% CI: 1.1–1.3; p<0.01), but have lower self-efficacy to quit (45.3% vs 50.1%, AOR=0.8; 95% CI: 0.7–0.9; p<0.01), compared to those without any of these conditions.
Among conditions with complex relationships with smoking, diabetes was associated with making more quit attempts, but not with any other quitting measures. Those reporting severe obesity were not only more likely to be currently abstinent, and report more quit attempts (for smokers), but were also more likely to plan future attempts. Chronic pain was associated with more quit attempts and use of quit medication, and overall negatively associated with self-efficacy to quit, where there was a significant by country interaction. There was a negative association in Canada (46.1% vs 58.2%; AOR=0.7; 95% CI: 0.5–0.9; p<0.05) and US (37.9% vs 49.8%; AOR=0.7; 95% CI: 0.4–0.9; p<0.05), but not in Australia or England.
Those who accepted that smoking had damaged their health were more likely to report having the specific health conditions; and those who perceived that smoking would damage health in the future were in most cases also more likely to have specific health conditions, except cancer, diabetes and severe obesity (Supplementary file, Table 2). Significant proportions of respondents with each of these conditions denied smoking had damaged their health and were not concerned about future adverse effects of smoking.
Those reporting that smoking had affected their health were more likely to be abstinent, made more quit attempts and plans for future attempts, but had lower self-efficacy (Table 2). There were significant by-country interaction effects for planning to quit. Those who accepted that smoking had damaged their health were more likely to plan to quit in Canada (50.4% vs 34.9%; AOR=2.0; 95% CI: 1.7–2.4; p<0.001), US (36.1% vs 29.5%; AOR=1.6; 95% CI: 1.2–2.1; p<0.01) and England (41.7% vs 32.9%; AOR=1.5; 95% CI: 1.2–1.9; p<0.001), but not in Australia (42.5% vs 39.3%; AOR=1.2; 95% CI: 0.8–1.7; p=0.31).
As in the case of reporting having been harmed by smoking, concern about future effects of smoking (among smokers only) was associated with more quit attempts and more future plans to quit. There was a significant by-country interaction between future concerns and self-efficacy to quit. Those with concerns were more likely to report lower self-efficacy in England (41.6% vs 53.3%; AOR=0.6; 95% CI: 0.5–0.7; p<0.001), but not in the other three countries. For neither general health concern measure (i.e. smoking had damaged or would damage health) was there any relationship with use of medications on their last quit attempt.
DISCUSSION
Overall, both general concerns about smoking damaging health and specific health conditions were associated with increased quit-related activity for at least one of the three measures used (being abstinent, quit attempts, and quit plans), except for alcohol problems. There was a general tendency for those with concerns, or conditions, to report lower self-efficacy for quitting, and while adjusted ORs for use of pharmacotherapy on last quit attempts were all above 1, most were modest and non-significant. There is cause for serious concern that smokers with medical conditions linked to their smoking are not much more likely to use evidence-based cessation medications. One would expect they are in regular contact with medical professionals who should be advising them about this and be better placed to obtain prescriptions required for some medications like varenicline, or which can result in a subsidized product for NRT in some places and circumstances. The common reports of lower self-efficacy indicate that the smokers, at some level, recognize the need for more help, but this is not translating into use of the best possible help. The levels of reporting quit activity were lower than might be expected, even allowing for memory effects, so the failure to find large differences in quit-related activities is probably not due to ceiling effects; that is, high levels of reporting among those without health problems.
We now discuss the results for various groups of health conditions in turn. First, the conditions strongly linked to smoking (heart disease, cancer, chronic lung diseases) when combined as a group, the results are consistent with what we had expected – having any of the three conditions was associated with greater quitting activities. Those with heart disease or cancer were more likely to be ex-smokers, suggesting it had motivated quitting, as found in many studies7,10,27, although it is surprising not to find this same relationship with chronic lung diseases. However, unlike the other two conditions, those with heart disease were no more likely to plan future attempts. Further, smokers with this group of conditions were no more likely to use cessation medications on their last quit attempts, and as mentioned above, there is cause for concern as people with such severe conditions should have been motivated by their health professionals to maximize the use of proven medications to quit smoking.
Moreover, that around one quarter of smokers with each of these conditions denied smoking had damaged their health is cause for real concern. Further, cancer patients were no more likely to be concerned about the future effects of smoking. While some of the cancers may not be related to smoking, probably most are, and continuing to smoke is likely to be more damaging. Perhaps some think all the harm has been done. The findings identify a failure by a minority to link smoking with having the illness. It is unclear whether this is due to health professionals failing to point it out, or some form of denial on the behalf of this minority or some combination of the two.
Next, considering the mental health conditions, the combined analyses indicate that those with any of these conditions report greater quitting activities, but this was not the case for alcohol problems when considered alone. Reporting alcohol problems was only found to be negatively associated with being abstinent, consistent with other studies2,14. Depression and anxiety were the two most commonly reported problems, and those reporting them were more likely to report recent (failed) attempts, consistent with existing research28, but had significantly lower self-efficacy, suggesting difficulties and challenges they faced to quit smoking2,17,18. It is also worth noting that daily smokers with these two mental conditions were more likely to use quit medications on their last quit attempts, while such positive associations were not found for other groups of conditions except for chronic pain.
Among the conditions with more complex relationships with smoking, diabetes is exacerbated by smoking29, so it is disappointing to see the relatively low level of belief that smoking had caused them harm and the lack of relationship with concern about future harm. While they were more likely to have reported quit attempts, they were not more likely to be ex-smokers and future plans to quit were also similar to those without the condition. The findings suggest a failure of diabetes education, but as we did not assess this, we cannot be sure if it was a failure to provide the information or resistance from the smokers to accept it.
Chronic pain has a complex relationship with smoking. Cigarette smoking may be both a cause of pain and a factor that sustains it30-32. Reporting chronic pain was positively associated with quit attempts and use of quit medications, however, again not the high rates expected if these individuals had an adequate understanding of the role of smoking in their condition. Smokers with chronic pain may benefit from quit medications to cope with the pain33, and indeed this was one group significantly more likely to use such products.
Severe obesity also has a complex relationship, as smoking cessation is associated with weight gain. Obesity was more common in recent quitters, which might be partly causal but also it is likely that those prepared to accept being overweight, as a lesser evil than smoking, were more likely to quit. This group also reported more plans and attempts to quit. Our findings are consistent with the work of others that do not find weight gain a barrier to successful quitting, even though worry about weight gain is often reported as a reason for not quitting34-36.
Smoking cessation treatment has been particularly challenging in some sub-populations, including among smokers with very limited financial resources to access pharmacotherapy that they need. Although some NRT products are subsidized by the governments in some jurisdictions (the subsidy varies in the four countries), many smokers are still struggling to cover the costs associated with NRT that is not subsidized. For example, in Australia, access to nicotine patches (for a 12-week period per year), under the Pharmaceutical Benefits Scheme (PBS), has been extended to all smokers since 2011, but a condition for the discount is that the smoker participates in cessation counseling37. Those who do not meet the condition and those who choose other forms of NRT need to pay for their quit medications.
Limitations
In interpreting the results, it is important to keep in mind that the ex-smokers in the study sample are all relatively recent ex-smokers, so, much of the quitting is likely to have occurred after the health problem was identified, but we do not know how much. This study depended on self-reported smoking status without biochemical validation, which is a limitation. Furthermore, as we mentioned earlier, some respondents were smokers and quitters who had responded to a previous ITC 4C Survey, and, compared to the newly recruited participants, may have had differential memory effects in reporting on quitting. One method to overcome the memory effect is to make use of more recent quit attempts38. We did ask about quit attempts in the past 12 months in this study, but we could not completely overcome the memory effect issue. We also acknowledge this cross-section analysis lacked an ideal control sample, although the original ITC 4C Survey had longitudinal and ‘quasi-experimental’ design features where ‘countries not implementing a given new tobacco control policy act as the control group to which the country implementing such a policy will be compared, provide much stronger evidence than observational studies on the effects of national-level tobacco control policies’23. This study has other limitations, including its cross-sectional design, which limits its capacity to demonstrate possible causal relationships. In some cases, causal associations have been established in other work, so we can be confident the increased quitting associated with heart disease, at least, is partly a result of being diagnosed with the condition. However, other associations require further work to understand them. The fact that mental health conditions, such as depression, were associated with increased interest in quitting but not to success in quitting is consistent with other work27 and highlights the additional difficulties such groups have in quitting successfully. Furthermore, there can be gaps between what respondents identify as having and what they actually have, which can be affected by level of education about their condition, the terminology used in the survey, and a range of other factors. These concerns do not lessen the importance of the findings. We expect that if a smoker is aware that his/her condition may be caused or worsened by smoking then this would be a critical element in motivating extra action.
CONCLUSIONS
While those with smoking related conditions are somewhat more aware of the links to their smoking, and are largely taking more action, the extent of this is lower than one might reasonably expect. More rigorous and targeted public health campaigns are needed to further raise the awareness of the harms of smoking among the public in general, and among those with various health conditions in particular. In the context of strengthened health promotion efforts, health professionals need to do more to use health conditions to motivate quit attempts and to ensure they are made with the most effective forms of cessation help.