INTRODUCTION
Tobacco use is recognized as a causative agent for head and neck (H&N) and lung cancers, but not for cancers of the prostate or breast. Still, tobacco use during radiotherapy has been associated with poorer outcomes for all four of these commonly treated malignancies1-6. Patients with these cancers who continue to smoke during radiotherapy have worse outcomes ranging from increased side effects during treatment to greater late effects including increased mortality from heart disease and second cancers. Active smokers also have inferior oncologic outcomes including poorer locoregional control, higher risk of developing distant metastases as well as decreased disease-free and overall survival.
While the literature is clear in showing the benefit of tobacco cessation for these four different cancers treated with radiotherapy, we questioned whether those tumors less commonly associated with tobacco causation (prostate and breast) underwent the same frequency of documentation and cessation discussion as patients with cancers more commonly associated with smoking (H&N and lung).
METHODS
This study was reviewed and approved by our IRB (study number IRB 16428). Initial consultation notes of 592 non-metastatic patients seen in a single academic radiation oncology department in Portland, Oregon USA from January 2014 through June 2017 were reviewed using the electronic medical record. These notes contained input from residents, attendings and nurses. Current smokers were identified as smoking up until the time of consultation with smoking status recorded in the consultation note. Discussions regarding smoking cessation were identified in the consultation treatment plan with offers of therapy including counseling and medicine. Descriptive statistics were used to evaluate smoking history and cessation discussions. SAS 9.4 (SAS Institute, Cary, NC) was used for statistical analysis. The chi-squared test was used to compare frequencies. A p-value <0.05 was considered to be statistically significant.
We chose two cancer sites commonly associated with tobacco use and causation (H&N and lung) and two sites not commonly associated (prostate and breast). We reviewed consultation notes of 135 H&N, 174 lung, 125 breast and 158 prostate cancer patients.
RESULTS
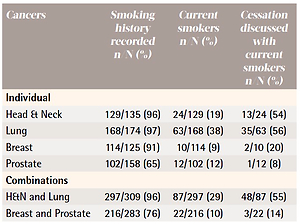
Prostate cancer patients were less likely to have their smoking history recorded at consultation (65%) than breast (91%), H&N (96%) or lung (97%) cancer patients (p<0.0001). Breast and prostate cancer patients were less likely to be current smokers (10%) than H&N and lung cancer patients (29%) (p<0.0001). Discussions regarding smoking cessation were less frequently documented in breast and prostate cancer patients (14%) than in H&N and lung cancer patients (55%) (p=0.0005). Table 1 gives the frequencies of smoking history documentation, current smoking status and our documentation of tobacco cessation discussions for the individual four sites as well as the combinations of H&N and lung, and breast and prostate cancers.
Table 1
Frequencies of smoking history documentation, current smoking status and documentation of tobacco cessation discussions for non-metastatic cancer patients for the individual four sites of malignancy as well as the combinations of H&N and lung, and breast and prostate, Portland, Oregon USA 2014–2017 (N=592)
DISCUSSION
Tobacco use during radiotherapy has been associated with poorer outcomes. Chen et al.1 reported worse outcomes in their actively smoking H&N squamous cell cancer patients including decreased overall survival, locoregional control, disease-free survival and higher late complication rate. Rades et al.2 found improved locoregional control in lung cancer patients who did not smoke during radiotherapy. The negative effects of smoking are not limited to cancers where tobacco is a known etiologic agent. Taylor et al.4 reported increased risk of developing lung cancer and higher cardiac mortality in smoking breast cancer patients receiving radiotherapy. Foerster et al.6 found that prostate cancer patients who were current smokers at the time of prostatectomy or beginning radiotherapy had higher risks of locoregional recurrence, developing distant metastases and increased cancer-specific mortality.
We did not record smoking history at initial consultation as frequently for prostate cancer patients than for the other three evaluated malignancies. It is possible that the overall low rate of prostate cancer patients who are current smokers affected this. Our 12% prostate cancer rate is lower than the Oregon adult smoking rate of 16.1% and the United States national rate of 17.1% during the period of this study7. We did a better job recording smoking history for our breast cancer patients even though this population had the lowest current smoking rate. Our H&N population approximated the Oregon and national smoking rates. Our lung cancer patients had a current smoking rate double the state or national overall smoking rates.
Overall, we do a poor job discussing smoking cessation with our current smoking cancer patients receiving radiotherapy. Even for smoking H&N and lung cancer patients, malignancies identified with tobacco causation, our discussion rate was only slightly better than half. We report an even lower effort with cessation discussions in the two cancers not commonly associated with tobacco use. Our results agree with those reported by Gallaway et al.8. Using data from the Kentucky Cancer Registry, these authors reported less common cessation counseling and medical intervention in non-tobacco-associated cancer survivors (including breast and prostate cancer) than in tobacco-associated cancers.
The reasons for lower rates of cessation discussions in our prostate and breast cancer populations are subject to speculation. Perhaps, we do not consider smoking cessation as important in malignancies not caused by smoking. Maybe we just do not think about smoking at all in these non-tobacco-associated cancers. Many providers may not be familiar with the literature showing poorer outcomes for current smoking breast and prostate cancer patients.
In any case, we need to do a better job identifying our radiotherapy patients who are current smokers. We need to do a much better job discussing cessation strategies and providing medical therapies for those patients interested in quitting. One strategy to improve these numbers involves use of the electronic medical record (EMR). Our department utilizes EMR for documentation and treatment planning including electronic prescriptions. We are exploring the possibility of ‘flagging’ current smokers’ consultations in the EMR and prohibiting completion of the visit encounter until the responsible provider acknowledges current smoking status and ‘signs off’ that tobacco cessation efforts were discussed.
Strengths and limitations
Patient number limits this review. Further, all these patients come from a single academic radiation oncology department where individual provider practice could have affected our findings. Still, the strength of this study is in identifying a problem. Specifically, we report lower rates of smoking cessation discussions in our breast and prostate cancer patients. The first step in improving this problem is to recognize that it exists.
CONCLUSIONS
We found a low rate of smoking cessation discussions in patients referred for radiotherapy who are currently smoking. We document smoking cessation discussions less frequently in current smoking non-tobacco-associated malignancies. These breast and prostate cancer patients make up a large portion of our academic radiotherapy practice. These non-tobaccoassociated cancer patients have inferior oncologic outcomes and higher morbidity if they continue to smoke during their radiotherapy. To improve outcomes in these patients, we need to do a better job of actively discussing tobacco cessation.