INTRODUCTION
Smoking is one of the most serious public health problems worldwide, and the World Health Organization (WHO) has drawn attention to the magnitude of the use of tobacco products by youth and adolescents1. Some alarming trends have been reported: both lifetime and current cigarette smoking are increasing steeply with age; and at the age of 11 years, 5% of boys and 2% of girls have ever smoked, rising to 29% of boys and 27% of girls by the age of 15 years1. Adolescence is a critical period when the risks associated with substance use are particularly high. Smoking behavior is typically established during adolescence; most smokers had their first cigarette or were already addicted by the time they turned 18 years. Compared with adults, young people require fewer cigarettes and less time to establish nicotine dependence1.
Hence, in addition to the importance of designing and implementing interventions to help smokers to quit, it is crucial to work towards limiting the initiation of the young into this addiction. Results for Spain from the 2011 European School Survey Project on Alcohol and Other Drugs (ESPAD)2, with more than 100000 students (aged 15–16 years) from 36 countries, showed that 35% of students had smoked tobacco once in their lifetime (30% boys, 40% girls), 19% in the previous 30 days, and 4% daily. Based on findings of the 2017 health survey published by the Spanish Ministry of Health3, 21% of the population aged ≥15 years reported smoking daily, 2.3% were occasional smokers, 24.9% were former smokers, and 50.7% had never smoked. Roughly 24% of the population aged ≥15 years were active smokers, with almost 1 in 4 Spaniards of that age reporting smoking. In the Survey on Drug Use in Secondary Education in Spain (ESTUDES 2018)4 of a representative sample of teenagers aged 14–18 years, tobacco was the most prevalent drug following alcohol: 41.3% had smoked tobacco at some point in their lives, and 26.7% reported tobacco use in the 30 days prior to the survey, with 9.8% reporting daily use in the last month. All of these percentages were higher than those from the previous 2016 survey.
Multiple smoking prevention programs for adolescents with different approaches, content, and mode of delivery have been proposed, but the evidence of their effectiveness is largely inconclusive5. Early education interventions in youth tobacco control were based on the ‘information deficit or rationale model’, in which the program provided information about the health risks and negative consequences of tobacco, mostly in a manner intended to arouse concern and fear6. Social learning theory suggests that adolescent smoking is a learned behavior acquired through social interactions and reinforcement7, and the sociopsychological strategy of deterrence is based on preventing children from starting to smoke8. These models, however, have not been successful in reducing the incidence of smoking in adolescence4. Multimodal programs are taking a step further beyond the school setting to intervene in the community, including families, the media, and legislative smoking bans, with a clear purpose of reducing secondhand smoke exposure and modifying the social environment in which tobacco consumption initiation occurs.
Although the school environment is one of the most suitable settings for preventing teenagers’ tobacco initiation and developing preventive programs, systematic reviews and meta-analyses have shown that school-based smoking programs have not influenced adolescent smoking behavior as much as anticipated9,10. A Cochrane systematic review of randomized controlled trials (RCTs) of incentive programs to prevent smoking uptake suggests that this strategy does not prevent smoking initiation among youth11. Also, behaviorally or psychosocially based adolescent smoking cessation interventions have produced only modest results12. A systematic review and meta-analysis of primary healthcare behavioral interventions for improving smoking outcomes for children and youth showed that the evidence on critical components of programs was limited by heterogeneity in methodology and intervention strategies13. RCTs of family interventions have shown mostly neutral or negative results14, and the evidence supporting Web-based interventions for smoking cessation in college students and adolescents is insufficient to moderate15.
We propose a multi-personal intervention model in which adolescent students, teachers, and parents are involved in optimizing smoking prevention strategies, considering individual and community environmental factors16. It is an intermediate proposal between social learning abilities and a complete multimodal program that combines a school-based intervention targeting students and teachers and a community-based intervention targeting the parents, but without actually incorporating the enforcement of legal norms. It is possible to carry out this intermediate proposal with the existing means of schools, without additional material or personal costs. Adapting the proposal to the school environment’s reality can help ensure its feasibility and practicality.
The study’s objective was to assess the effectiveness of this multi-personal intervention model based on actions for students, teachers, and parents to prevent tobacco use among adolescents in secondary education.
METHODS
Design and setting
An analytical quasi-experimental and non-randomized study was carried out among secondary school students, aged 12–17 years, who attended first, second, and third grades of compulsory secondary education (Educación Secundaria Obligatoria, ESO) at the Joan Fuster High School in the city of Sueca (27640 inhabitants) located in the autonomous community of Valencia, Spain. Sueca is the capital of the Ribera Baja region (Southern Valencia). It has the largest high school where compulsory secondary education, baccalaureate, automotive maintenance, and administrative training cycles are taught. The total number of students is around one thousand. The study was carried out during the 2017–2018 academic year.
The study’s objective was to assess the effect of a multi-personal intervention model, with specific actions addressed to students, parents, and teachers, on the reduction of tobacco consumption by adolescents. It was hypothesized that providing extensive information on smoking-related health consequences would reduce adolescent smokers’ prevalence one year after the intervention. The multi-personal intervention (intervention group) was compared to standard anti-smoking activities carried out regularly by the local government administration to prevent the initiation of tobacco use at the general level of high school students (control group) of the autonomous community.
Sample size and participants
The sample size was calculated according to a rate of smoking in the last 12 months of 34% in the control group based on data from the ESTUDES 2016–2017 survey4 and assuming a 20% rate in the intervention group, with an alpha level of 0.05 and 80% statistical power, giving a total of 141 students per group necessary. This number was increased to 148 participants per group, assuming 5% losses to follow-up.
Students, parents, and teachers of the 14 classes of the 1st, 2nd, and 3rd ESO grades were eligible to participate in the study. Given that recruitment of parents of the intervention group would be expected to be more complicated than the recruitment of students and teachers, it was decided to take advantage of the informative meetings with tutors of each ESO class, which take place at the beginning of the academic year and are attended by most of the parents, to conduct the intervention with parents before the meeting with the tutor. The criterion of opportunity was chosen when selecting the assignment of parents to the intervention or the control groups, as the schedules of the different tutors’ meetings overlapped in some of the 14 classes of the 1st to the 3rd ESO grades. Based on the availability of non-coinciding schedules to carry out the intervention activity, the students whose parents had attended the intervention workshop were chosen to be included in the intervention group. Approximately half of the parents were selected for the intervention group and the other half for the control group. The assignment of students to the intervention group was conditional on the intervention having been previously conducted with their parents.
Eligibility criteria for students were: aged 12–17 years, enrolled in 1st, 2nd, and 3rd ESO grades at the Joan Fuster High School of Sueca city during the 2017–2018 academic year, with expectations of continuing studies at the high school for at least one more year. Students for whom written informed consent was not obtained were excluded from the study. Eligibility criteria for parents were as follows: being a parent of a student included in the intervention group, attending a workshop on tobacco prevention (intervention group), signing the consent form to participate in the study, and signing the consent form for the inclusion of their child in the study.
Study procedures
At the beginning of the 2017–2018 academic year, parents in the intervention and control groups were provided with an informative brochure that included explanations of what parents can do to protect children from tobacco smoke and how they can act as models to encourage non-smoking initiation and support smoking cessation among adolescents who smoke. Also, all parents completed a simple questionnaire on smoking habits. The parents of the intervention group received a 50-min talk delivered by the tutors focused on extensive information on the consequences of tobacco use and passive smoking, new nicotine delivery devices and electronic cigarettes, and parents’ role in favoring smoking cessation/reduction of their children.
All teachers completed a baseline questionnaire on smoking habits. The intervention with the teachers was focused on three points: teachers’ exemplary role concerning smoking in front of their students, information about new nicotine delivery devices and electronic cigarettes, and information about websites and resources with scientifically proven reliable evidence on tobacco prevention in adolescents.
Students in both the intervention and control groups participated in a 60-minute workshop conducted by a psychologist of the Community Prevention Unit of the Sueca city council, in which the following contents were developed: 1) What is a drug and how are drugs classified?; 2) Components of tobacco; 3) Effects of tobacco consumption; 4) Short-term and long-term health risks associated with smoking; 4) Concepts of dependence, tolerance and withdrawal syndromes; and 5) Tobacco abuse, current smoking situation, and myths about smoking. In addition, all students, both in the intervention and the control groups, completed an ad hoc questionnaire with general aspects on age, sex, school year, being a repeater or not of any academic year, the student’s cigarette smoking history, attitudes towards cigarette smoking, alcohol consumption, and passive cigarette smoking. The details of this questionnaire which was anonymous, self-administered, and completed by students in their classrooms without the presence of teachers, have been previously reported17.
Students in the intervention group developed two activities throughout the course and during the tutoring hours, both of which aimed at the following: 1) enhance protective factors and the reduction of risk factors for smoking involving the students individually and their peer groups, 2) strengthen social skills to quit, and 3) managing social influence towards tobacco consumption. The first activity was a 50-minute talk by the principal investigator (JAR-O) on various aspects of tobacco use and the importance of not smoking. The second activity was led by the tutors. It included viewing videos selected for this purpose created by different organizations/ entities (e.g. Valencian Department of Health, Spanish Association Against Cancer, Zaragoza City Council). When a critical topic to be addressed appeared in these videos, a pause was made, and a discussion was initiated about the point that should be emphasized to the adolescents. Also, an interactive activity through the website www.drojnet.eu was developed, where attractive images were used to provide teenagers with accurate, simple, and age-appropriate information about tobacco prevention and consumption.
One year after the intervention (at the beginning of the 2018–2019 academic year), all participants self-completed an anonymous questionnaire to assess the change in their smoking status. Table 1 summarizes the characteristics of the study.
Table 1
Summary of the characteristics of the study
The level of nicotine dependence was assessed with the Fagerström test for nicotine dependence, a 6-item self-reported questionnaire that evaluates the quantity of cigarette consumption, the compulsion to use, and dependence. The items are summed to yield a total score of 0 to 10. Subjects were instructed to focus on the previous month when completing the questionnaire. Standard cut-off values for dependence are: <4, low; 4–6, moderate; and >7, high. A Spanishvalidated version was used18.
Data collection
Pre-intervention data included age, sex, ESO grade, smoking status, age started smoking, being a repeater or not of any academic year, alcohol consumption, nicotine dependence, parents’ and teachers’ smoking status, and changes in tobacco use after the intervention.
Statistical analysis
Categorical data are expressed as frequencies and percentages, and continuous data as mean and standard deviation (SD), or median and interquartile range (IQR: 25th–75th percentile). Categorical data were compared with the chi-squared test and quantitative data with Student’s t-test. To assess the effectiveness of the intervention, an ordinal regression model and a linear mixed-effects model were fitted, taking into account the group (intervention, non-intervention), time (before and after intervention), and the student (as a random factor). Odd ratios (ORs) and 95% confidence intervals (CIs) were estimated. Statistical significance was set at p<0.05. All statistical analyses were performed with the R statistical package (version 3.6.1.) and the ordinal (2019, 4–25) and clickR (0.4.32) packages.
RESULTS
Study population and baseline data
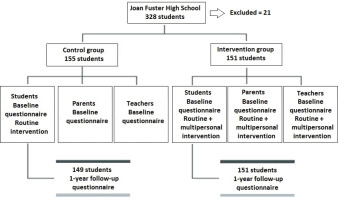
During the 2017–2018 academic year, there were a total of 328 students attending 1st, 2nd, and 3rd ESO grades at Joan Fuster High School, but 21 were excluded from the analysis. Eleven students were absent during the days on which the study procedures took place, and 11 provided incomplete questionnaires. Therefore, the study population included 306 students; 151 were assigned to the intervention group and 155 to the control group. A total of 41 teachers participated in the study. At the beginning of the 2018–2019 academic year, the follow-up questionnaire at 1 year was completed by the 151 students from the intervention group and 149 students from the control group (since six students assigned to this group were absent). The flow chart of participant selection is shown in Figure 1.
The general characteristics of students in the intervention and control groups are shown in Table 2. In all, 50.3% of students were boys, and 49.7% were girls, with a mean age of 13.4 years. About one-third of students were repeaters. Thirty-six students (21 in the intervention group and 15 in the control group) were current smokers, with a smoking prevalence rate of 11.8%. The mean (SD) age started smoking was 12.6 (1.6) years, without significant differences between the study groups. Never smokers accounted for 69.9% (n=214) of the population, and ex-smokers for 18.3% (n=56). The percentage of smokers among girls was 58.3% (n=21). Twenty-two smokers (61.1%) reported weekly consumption, 7 (19.4%) smoked between 1 and 10 cigarettes daily, 6 (16.7%) were occasional smokers (<1 cigarette/week), and only 1 (2.8%) smoked >10 cigarettes/day. The percentage of smokers aged 13–14 years was 63.9% (n=23), higher than 30.6% (n=11) found for those aged 15–16 years. The level of nicotine dependence was low/moderate in 34 smokers (94.4%). The peak of smokers of 44.4% (n=16) was observed at 14 years of age.
Table 2
Demographic and general descriptive characteristics of the study population within this quasi-experimental study, Spain
| Characteristics | Control group (N=155) n (%) | Intervention group* (N=151) n (%) |
|---|---|---|
| Sex | ||
| Boys | 80 (51.6) | 74 (49.0) |
| Girls | 75 (48.4) | 77 (50.9) |
| Age (years), mean (SD) | 13.4 (12.1) | 13.5 (0.9) |
| Age started smoking (years), mean (SD) | 12.7 (1.5) | 12.6 (1.6) |
| School grade | ||
| 1st | 89 (57.4) | 24 (15.9) |
| 2nd | 31 (20.0) | 81 (53.6) |
| 3rd | 35 (22.6) | 46 (30.5) |
| Repeaters (students enrolled in a class for the second time) | 51 (32.9) | 41 (27.1) |
In relation to the consumption of alcohol and tobacco (Table 3), 66.8% (n=183) of students who reported that they did not consume alcohol were non-smokers versus 25% (n=9) among smokers. Occasional alcohol consumers or those who reported to consume alcohol when they went out partying and smoked, accounted for 69.3%, compared to sporadic drinkers or non-smokers when they went out partying, who accounted for 32.2%.
Table 3
Alcohol consumption and tobacco use among participants in the quasi-experimental study, Spain
| Alcohol consumption | Non-smokers (N=270) n (%) | Smokers (N=36) n (%) |
|---|---|---|
| Daily or almost daily | 0 | 2 (55.5) |
| Occasionally | 55 (20.4) | 14 (38.9) |
| Only when going out partying | 32 (11.8) | 11 (30.5) |
| Never | 183 (67.8) | 9 (25.0) |
Smoking status among parents included 64 (42.4%) smokers in the intervention group and 46 (29.7%) in the control group. In the group of 41 teachers, daily and occasional smokers accounted for 19.5% of cases (n=8), ex-smokers for 34.1% (n=14), and never smokers for 46.3% (n=19).
Data at follow-up at 1 year
All 151 students from the intervention group and 149 from the control group (96.1%) completed the follow-up questionnaire after one year, at the beginning of the 2018–2019 academic year. Changes in smoking status are shown in Table 4. The percentage of non-smokers increased from 84.1% to 88.7% in the intervention group. In contrast, it remained almost unchanged among the controls (89.3% vs 89.9%). There was an increase in the prevalence of non-smokers of 4.6% and a decrease in the prevalence of smokers of 4.7% among students who received the multi-personal intervention, as opposed to the control group, where the prevalence showed a 0.6% decrease.
Table 4
Changes in smoking status in the intervention and control groups at follow-up at 1 year, within this quasi-experimental study design, Spain
The regression analysis showed that the multi-personal intervention had a positive effect on the prevention of smoking. The students who received the intervention smoked less or quit smoking more than those in the control group (OR=0.135; 95% CI: 0.019–0.973, p=0.047).
DISCUSSION
Despite the large number and variety of interventions carried out in the school environment to prevent tobacco initiation, the high tobacco consumption among adolescents in Spain continues to be a growing concern4. In this study, a multi-personal intervention applied to 306 secondary school students was associated with a significantly higher percentage of students who smoked less or quit smoking than the control group at follow-up at 1 year. Development of the multi-personal model was feasible and did not require financial resources. Numerous studies on the prevention of tobacco consumption in adolescents, most of them targeting the students themselves, have shown discouraging or mixed results19-25. A systematic review and meta-analysis of 11 studies and 6469 adolescents showed a high overall prevalence (41%) of adolescents in the pre-contemplation stage (Transtheoretical Model) who displayed more unfavorable smoking-related behavior than adolescents in other stages26. In a meta-analysis of different smoking prevention programs for young adolescents based on 23 RCTs, no significant effects were found for family-centered or web-based programs, with the most effective being those conducted by a trained teacher and in a school setting27. However, in a study carried out in 22 secondary schools from Spain with 1055 students (aged 12–13 years) enrolled in 2 successive cohorts from 2010 to 2011, a teacher-delivered school-based intervention on the initiation of smoking was not effective at follow-up at 3 years after the intervention25.
However, the results of interventions that include school-based programs, reinforcement of a smoke-free school policy, smoking cessation for teachers, brochures for parents, and other community-based activities involving youth clubs and tobacco sales, endorse the effectiveness of multimodal smoking prevention programs, which include strategies with adults who influence adolescents28. Short-term results (12 months) of the European Smoking Prevention Framework Approach (ESFA) to prevent smoking onset with a total sample of 15422 students from six countries showed different results, with fewer non-smokers starting to smoke weekly in the experimental groups versus controls in Finland and Spain. However, counter-productive effects were observed in Denmark and the UK29. At follow-up at 24 and 30 months, smoking onset was 36% lower in the experimental group in Portugal, 15% in Finland, and 12% in Spain. In contrast, in The Netherlands, the ESFA program was effective for non-native adolescents, with 11.4% new weekly smokers compared to 19.9% in the control group, and the opposite effect in native Dutch adolescents30. Although the ESFA project targeted four levels, i.e. adolescents in schools, school policies, parents, and the community, a better assessment of which elements are responsible for behavioral effects is necessary.
A study by Gómez Cruz et al.22 involved a 3-year smoking intervention program for students in secondary education from two institutes, one in Zamora and another in Salamanca. The program using the ESFA project questionnaire included prevention and treatment activities, and in the conclusions, three critical aspects were highlighted, which have been addressed in the present study. When developing a tobacco consumption prevention program for adolescents, clinical criteria should be replaced with pedagogical standards, the program’s intensity should be reduced, started at earlier ages, and parents should be involved. These three suggestions have been considered in the design of the present multi-personal intervention model.
The overall prevalence of smoking was 11.8% (13.9% in the intervention group and
9.8% in the control group), which coincides with the prevalence reported in the ESFA project in a sample of 1952 1st-grade ESO students from 53 schools in Barcelona31. In our study, of the 36 students who were smokers, 8 (22.2%) reported smoking on a daily basis, a percentage higher than 10.4% of daily smokers in the last 30 days reported in a survey study of 2412 school-aged adolescents aged 13–18 years in the province of Valladolid, Spain32, as well as higher than 9.8% found in the ESTUDES 2018–2019 survey4. Interestingly, the mean age at initiation of cigarette smoking was around 13 years. Data collected from the Global Youth Tobacco Survey (GYST) 2010–2020 in 144 countries for a total of 432969 adolescents, the highest proportion of cigarette smoking initiation (36.8%) was at age 12–13 years, followed by 14–15 years (21.6%), and the average age of cigarette smoking initiation decreased or remained unchanged in nearly three-quarters of the countries surveyed33. In a previous GYST study on adolescents aged 12–16 years, comprising 456634 participants from 147 countries between 2006 and 2018, the age started cigarette smoking was 10.7 years for girls, significantly earlier than 11.8 years for boys, in low-income countries. The average percentage reported by those who started smoking at an age <12 years was 58.1% in lower middle-income countries compared to 41.8% in high-income countries34. All these findings emphasize that intervention strategies and measures aimed at children to prevent smoking uptake, should be a key public health priority worldwide. Moreover, the vital role played by gender in adolescent smoking behavior35, with higher proportions of smokers among girls (58.3% in our study), may support the development of gender-tailored smoking prevention and cessation interventions.
Although school-based and community interventions with a control group should be designed as randomized studies19, allocating randomly to the experimental or control conditions is challenging to implement in practice. In the ESFA project, randomization of experimental and control regions was feasible in only three of the six participating countries20. In other studies where randomization was performed, substantial differences in baseline data between the study groups were observed21,36. In our research, allocating students to the control or intervention groups was done based on a previous selection of parents attending pre-course tutoring meetings and the opportunity criterion of overlapping tutorial sessions to assign them to an intervention workshop or a control group. As a result, all students from the different classes of 1st, 2nd, and 3rd ESO grades were included in one of the two study groups, which were homogeneous regarding the main baseline variables.
Limitations
The present study should be interpreted considering its potential limitations, such as the selection of a convenience sample from a single high school, the use of electronic cigarettes or biomarkers of tobacco exposure were not evaluated, and the short duration of the intervention. Also, psychosocial characteristics and risk factors for adolescent smoking uptake (e.g. ethnicity, family structure, parental socioeconomic status, attachment to family and friends, siblings/ friends smoking status, risk behaviors, social media use, etc.) were not recorded but could have also impacted the results in any direction. On the other hand, it would have been interesting to perform a sensitivity analysis by breaking down participants by class or gender.
CONCLUSIONS
The multi-personal model developed in this study with the participation of teachers and parents was feasible, and the intervention led by training teachers was simple to implement. After one year, there was an increase in the prevalence of non-smokers of 4.6% and a decrease in the prevalence of smokers of 4.7% among students who received the multi-personal intervention. By involving parents in the preventive model, we incorporated the adolescent’s family environment, thus emphasizing their contribution as role models and expanding efforts to the family setting to prevent the initiation of tobacco use.