INTRODUCTION
According to the World Health Organization, the United States ranks second in global surgical volume, with over 36 million surgeries performed each year as of 20121. The prevalence of tobacco use among the US surgical population is disproportionately high, with estimates suggesting that 30% of patients undergoing elective general surgery are active smokers2. Preoperative smoking is an independent risk factor for significant postoperative morbidity and mortality3-5.
Recent analyses suggest smokers are up to 1.53 times more likely to die in the 30 days after surgery than non-smokers6. Preoperative smokers also experience higher rates of postoperative pneumonia, post-surgical intubation, myocardial infarction, stroke, sepsis, and wound complications than both non-smokers and former smokers3-5,7. The added burden posed by smoking on both perioperative patients and the health system has been described across surgical disciplines, leading the American College of Surgeons to declare that smoking cessation counseling should be offered during all non-emergent patient consultations6.
Among US smokers, 68% report wanting to quit completely7. Despite patient interest and proven postoperative risks, only 58% of surgeons ‘almost always’ advise their patients who use tobacco to quit. Moreover, only 13% of surgeons ‘almost always’ provide resources to help their patients who use tobacco to quit8. Surgical clinics pose an exceptional opportunity to encourage behavior change, with studies demonstrating that the experience of scheduling elective surgery produces a significant, actionable incentive to stop smoking2,9.
Clinical decision support (CDS) is a system in which physicians are provided with knowledge that is intelligently filtered and presented at appropriate times to enhance healthcare delivery10. CDS systems may include computerized alerts and reminders, condition-specific order sets, and contextually relevant reference information10,11.
A CDS tool was designed to increase smoking cessation counseling referrals among patients seeking elective surgery at the James J. Peters VA Medical Center (JJP-VAMC) with a secondary objective to assess the utilization rate of this referral system.
METHODS
Design and setting
This was a pretest-posttest study of a CDS tool created in the VA electronic medical record, Computerized Patient Record System (CPRS). The study was managed by the Preventive Medicine Department at the JJP-VAMC and attached to both plastic and vascular surgery clinic notes from July 2019 to February 2020. This CDS tool was designed as a low-click, streamlined means of referring patients to available smoking cessation clinics at the facility. The study was classified as a quality improvement project per VA guidelines and was approved for use in all patients seen in plastic and vascular surgery clinics.
Intervention
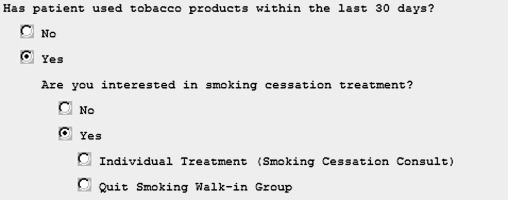
An electronic CDS tool was implemented to assess smoking status and desire for treatment at the initiation of plastic and vascular surgery clinic notes. It was designed as a series of three conditional statements to facilitate ease of use. ‘Treatment’ referred to the multiple treatment modalities offered at JJP-VAMC, including either a smoking cessation clinic appointment, where counseling as well as pharmacologic therapies are offered, or weekly support groups. The tool included the following questions: 1) ‘Has the patient used tobacco products within the last 30 days?’, 2) If ‘yes’, ‘Are you interested in smoking cessation treatment?’ and 3) If ‘yes’, the clinician would choose ‘individual treatment’ or ‘group therapy’ (Figure 1). By clicking ‘individual treatment’, the prompt would generate an automatic, pre-populated referral order, with the provider responsible only for providing a suggested consultation date. If ‘Quit Smoking Walk-In Group’ was selected, the tool displayed a printable flyer. If ‘no’ or ‘cancel’ was selected at any time, the template would close with no further actions required. A ‘cancel’ button was found at the bottom of each screen of the tool and could be selected at any time. The tool was designed to record all inputs and premature cancelations.
Figure 1
CDS tool (first screen). This image is the first screen of the CDS tool that appeared when a consultation note was created. The tool was designed to minimize interactivity (mouse clicks), provide only the essential information needed to refer a patient to smoking cessation services, and limit time spent in the tool (reading/clicking) by the clinical user. The following screen (not displayed) allowed placement of a pre-populated referral order
Samples
The pretest sample group was defined as the number of referrals to smoking cessation services made by plastic surgery and vascular surgery clinics from June 2018 to June 2019. The posttest sample group was defined as the number of referrals to smoking cessation services using the CDS tool throughout the implementation period. These de-identified data were accessed via the JJP-VAMC Department of Medical Informatics.
Implementation
The first phase of implementation ran from July to November 2019 when the tool was implemented in the plastic surgery clinic only. This clinic had lower volume and therefore served as a pilot environment to assess barriers to CDS deployment before expanding to the larger vascular surgery clinic. The second phase ran from November 2019 to February 2020. This phase saw an expansion of the tool to notes in vascular surgery clinics with continued use by plastic surgery.
RESULTS
A pretest data request of plastic and vascular surgery clinic consultations revealed that zero patients were referred to smoking cessation clinics over the 12 months before study implementation. This encompassed 278 and 564 eligible consultations, respectively. Posttest examination demonstrated that for the plastic surgery clinic, between July 2019 and February 2020, a total of 201 new patient consultations were completed. Providers utilized the CDS tool for 191 (95.0%) patients, with 10 patients (5.0%) bypassed by providers clicking cancel on the collection instrument. Of the 191 patients, 160 (83.7%) were noted to be non-smokers and 31 (16.3%) were active smokers. Twenty-six of the smokers (83.9%) refused treatment, and five smokers (16.1%) accepted individual treatment with a referral to the smoking cessation clinic.
Within the vascular surgery clinic, a total of 195 new patient consultations were completed between November 2019 and February 2020. For the 195 consultations, providers utilized the CDS tool for 98 (50.3%) patients, with 97 patients (49.7%) bypassed by providers clicking cancel on the collection instrument. Of the 98 patients, seventy-five (76.5%) were noted to be non-smokers, 10 (10.2%) were logged as active smokers, and thirteen (13.3%) additional patients were lost due to cancelation after initiating data entry. Of the identified smokers, the element was canceled for two (20%), five (50.0%) refused treatment, and three (30.0%) accepted individual treatment with a referral to the smoking cessation clinic. Comparing pretest and posttest values using a one-tailed Z-test, CDS tool implementation produced a significant increase in referrals for both plastic (p=0.00415) and vascular (p=0.00159) clinics.
DISCUSSION
The purpose of this study was to examine the effectiveness and utilization rate of an electronic CDS tool designed to improve referral rates to smoking cessation services in outpatient surgical clinics. The CDS tool successfully improved the incidence of smoking cessation referrals in two surgical clinics from pretest baselines. These clinics had referred zero patients to smoking cessation services in the year before implementation. In the eight months during which tool use was measured, they collectively referred eight smokers to cessation services. Utilization rates varied between surgical clinics, with frequencies of 95.0% in the plastic surgery clinic and 50.3% in the vascular surgery clinic.
Limitations
This study had limitations. First, CPRS required that the tool automatically open when a new patient consultation note was generated. Surgeons endorsed that they typically assess smoking behavior later in the course of patient interviews. The timing of the CDS tool pop-up was dyssynchronous with the optimal workflow of the clinical visit, and the tool did not trigger again if canceled. Moreover, the CDS tool was not mandatory to acknowledge. Both vascular and plastic surgery clinics are high-volume, time-pressured environments, where disruptions in clinic pacing can be detrimental. These factors likely contributed to cancelation rates; CDS tools not integrated into the clinical workflow and not mandatory to acknowledge are more likely to be overridden12,13. Next, data was limited to plastic and vascular surgery clinics, which may impact the generalizability of these results to all outpatient surgical clinics. Additionally, though utilization rates are a reasonable predictor for feasibility, further qualitative data on provider’s opinions of tool usability could have informed optimization of the instrument. Finally, multiple attempts to provide education regarding tool use were provided to the vascular clinic, but this was not feasible due to scheduling. Cancelation is presumably the cause behind the low percentage of vascular patients identified as smokers.
Despite receiving no formal education on CDS tool use and the aforementioned limitations, the observed utilization rate among vascular surgery residents and attendings was 50.3%, a value in line with successful utilization reported in CDS literature12-17. The plastic surgery clinic achieved a 95.0% utilization rate following directed education, suggesting there is potential for significant uptake by surgical providers.
The VA health system is a unique environment to test CDS tools aimed at facilitating smoking cessation as VA Directive 1056 states that all facilities must provide patients with opportunities for behavioral counseling and pharmaceutical assistance in quitting smoking18.
CONCLUSIONS
This study demonstrates that a simple CDS tool can significantly improve referrals by outpatient surgical providers to smoking cessation services. Our preliminary data strongly suggest that future studies should examine the efficacy of expanding comparable CDS tools among outpatient surgical clinics, as these tools enable the preoperative visit to serve as a more impactful opportunity to encourage smoking cessation.


