INTRODUCTION
Pediatric tobacco smoke exposure (TSE), defined as involuntary exposure to secondhand and thirdhand smoke1, is estimated to contribute to over 101000 excess emergency department (ED) visits resulting in an additional $63 million in TSE-related healthcare costs each year2. Over five million annual ED visits in the US among children aged <15 years are linked to complaints potentially related to TSE including cough, congestion, and earache3. While cigarette smoking rates among the adult population nationwide just hit a record low4, rates remain disproportionally high among parents of Pediatric ED (PED) patients 5. Parental smoking is an important source of child TSE, through both secondhand and thirdhand smoke1; cessation is the only way to fully protect children from this exposure source6,7.
National recommendations encourage adult tobacco use screening and cessation counseling in healthcare settings8-10. Despite available evidence-based clinical interventions to promote smoking cessation among adults, there remains room for improvement in the implementation of such efforts11. Approximately 43% of US adult smokers did not receive advice to quit smoking during their healthcare visits in 201511. Consequently, increased smoking rates exist among adult smokers who are racial/ethnic minorities and with lower socioeconomic status11. These disparities have been recently observed among children with TSE nationwide12, and among those who seek treatment in the PED/Urgent Care (UC) at the children’s hospital where the present study was conducted13. Unfortunately, tobacco screening and cessation counseling remain nascent in the current study’s acute healthcare setting, with prior qualitative work among PED practitioners citing reasons such as lack of time and resources, and competing acute care demands14. Despite parents reporting approval of cessation interventions during their child’s visit, nearly one in two PED patients who present to this children’s hospital do not undergo screening for TSE15, and rates of advising parents to quit smoking are much lower16.
PED/UC visits have been deemed a ‘teachable moment’ for providing parents with smoking cessation counseling5,17. ED-initiated tobacco control efforts are beneficial and promote tobacco abstinence among hard-to-reach adult smokers18. Prior research indicates PED/UC healthcare professionals at this children’s hospital generally have positive attitudes towards screening and advising parents to quit smoking14,19. However, the current lack of screening and intervention suggests the need to gain insight from PED/UC healthcare professionals to lay the groundwork for developing and implementing a sustainable TSE reduction intervention in this setting. Findings from this pilot study may also be used by researchers and practitioners in other PED/UC settings.
The present study sought to assess current tobacco screening and cessation counseling practices offered in the PED/UC to parents of pediatric patients at one large, Midwestern children’s hospital. We identified current practices of performing the 5 As of tobacco counseling (Ask, Advise, Assess, Assist, and Arrange), as outlined by the U.S. Public Health Service’s9 Clinical Practice Guideline for Treating Tobacco Use and Dependence, among PED/UC nurses and physicians. Secondarily, we assessed several factors associated with performing TSE reduction and tobacco cessation counseling in the PED/UC at this children’s hospital.
METHODS
Participants
We conducted a descriptive, cross-sectional pilot survey among a stratified purposive sample of 30 PED/UC nurses and physicians working at one large, Midwestern children’s hospital.
Measures
Please refer to Supplementary file Table 1 for the survey items asked among our population by adapting questions from established instruments20, including the American Academy of Pediatrics (AAP) Periodic Survey on Tobacco (No. 78)21. We assessed: current practices of performing the 5 As of tobacco counseling; perceived level of confidence in tobacco counseling; perceived levels of ease, effectiveness, optimism, and preparedness in tobacco counseling; perceived level of importance of tobacco counseling; perceived barriers to tobacco counseling; clinical practice and hospital environmental factors related to tobacco counseling; perceived patient TSE levels; and professional position and demographic characteristics including tobacco use status. Similar to work by the AAP21, and based on our skewed data, we collapsed the scale response options into two categories (Supplementary file Table 1).
Table 1
PED/UC healthcare professionals’ demographic characteristics, position characteristics, and clinical practice and hospital environmental factors related to tobacco counseling
| Characteristics | n (%) a |
|---|---|
| Demographic characteristics | |
| Age (years), mean (SD) | 42.1 (10.1) |
| Sex | |
| Male | 5 (16.7) |
| Female | 25 (83.3) |
| Race/ethnicity | |
| Non-Hispanic White | 28 (93.3) |
| Non-Hispanic other/unknown | 2 (6.7) |
| Education level | |
| College graduate/some post-college | 10 (33.3) |
| Master’s degree | 8 (26.7) |
| MD/DO | 12 (40.0) |
| Tobacco use status | |
| Never user | 26 (86.7) |
| Former user | 3 (10.0) |
| Unknown (did not wish to answer) | 1 (3.3) |
| E-cigarette use status | |
| Never user | 30 (100.0) |
| Position characteristics | |
| Position | |
| Nurse | 18 (60.0) |
| Physician | 12 (40.0) |
| Work hours/week, mean (SD) | 34.6 (10.9) |
| Patients cared for/week, mean (SD) | 49.9 (33.9) |
| Years in current position, mean (SD) | 8.0 (8.3) |
| Years at the hospital in any position, mean (SD) | 13.9 (8.4) |
| Clinical practice and hospital environmental factors related to tobacco counseling | |
| Estimated percentage of PED/UC patients exposed to secondhand smoke, mean (SD) | 43.6 (21.9) |
| Has system for routinely screening patients for secondhand smoke exposure | |
| No | 19 (63.3) |
| Yes | 5 (16.7) |
| Don’t know | 6 (20.0) |
| Hospital has EMR reminders to advise parental smokers to quit smoking | |
| No | 10 (33.3) |
| Yes | 3 (10.0) |
| Don’t know | 17 (56.7) |
| Hospital should have tobacco cessation plan or counseling service referral for parental smokers | |
| No | 1 (3.3) |
| Yes | 27 (90.0) |
| Don’t know | 2 (6.7) |
| Aware of the Clinical Practice Guideline (i.e. the 5 As) | |
| No | 22 (73.3) |
| Yes | 3 (10.0) |
| Don’t know | 5 (16.7) |
| Received training on tobacco counseling, past 12 months | |
| No | 27 (90.0) |
| Yes | 1 (3.3) |
| Don’t know | 2 (6.7) |
Procedures
We used PED/UC listservs to invite nurses and physicians with direct patient contact to participate in this study. An email invitation was sent to 297 nurses and 76 physicians. We used a stratified purposive sampling design to ensure both nurses and physicians were represented in the recruited sample. Interested participants emailed study staff. We sent study information along with a personalized link to a Qualtrics online survey. Participants reviewed the study information sheet and provided informed consent in Qualtrics. Participants then completed the survey adapted for healthcare professionals working in the PED/UC setting. Qualitative interviews were conducted after survey completion. Following standard recommendations for conducting qualitative research22, saturation was determined to be reached when no new information emerged from participant interviews. Therefore, survey study participation was capped at the first 30 participants. The current study focuses exclusively on quantitative survey results to explore current tobacco counseling behavior to potentially inform future intervention research at the children’s hospital. Participants were eligible if they were currently employed in the PED/UC and had direct patient contact at the time of survey completion. This urban, freestanding tertiary care hospital has about 1.2 million annual patient encounters overall, and >150000 visits are at the two PED and five UC sites. Participants were offered a $50 payment after completing all study activities.
Statistical analysis
We calculated descriptive statistics for current practices of performing tobacco counseling, attitude and practice factors, and participant characteristics. We also conducted a series of chi-squared tests to measure several factors (e.g. perceived barriers) that were associated with healthcare professionals’ performing tobacco counseling. We used R version 4.0.0., with level of significance set at 0.05.
RESULTS
Participants’ mean (SD) age was 42.1 (10.1) years. Most were non-Hispanic White (93.3%) followed by non-Hispanic other or unknown race (6.7%). About 87% of participants never used tobacco and 100% never used e-cigarettes. Sixty percent were nurses and 40% were physicians who worked a mean (SD) of 34.6 (10.9) hours/week and cared for a mean (SD) of 49.9 (33.9) patients/week. Participants worked an average (SD) of 8.0 (8.3) years in the PED/UC, and 13.9 (8.4) years at the hospital in any department (Table 1).
Clinical practice and hospital environmental factors related to tobacco counseling
Participants estimated that 43.6% (SD=21.9) of PED/ UC patients were exposed to secondhand smoke. Most (90%) participants thought the hospital should have a tobacco cessation counseling plan or counseling service referral for parental smokers. However, 90% had not received any training on tobacco counseling in the past 12 months, and nearly three-quarters (73.3%) were unaware of the Clinical Practice Guideline (i.e. the 5 As). Additionally, 63.3% did not have a standardized system for routinely screening for secondhand smoke, and 56.7% did not know whether the hospital’s electronic medical record (EMR) system had prompts for advising parental smokers to quit smoking.
Current practices of performing the 5 As of tobacco counseling
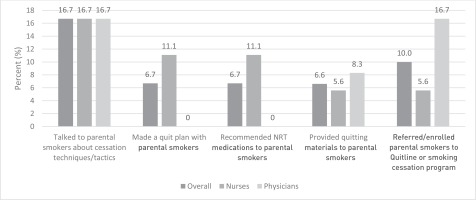
Figure 1 shows PED/UC healthcare professionals’ current practices of the performing the ask, advise, and assess steps. Figure 2 shows the current practices of performing the assist and arrange steps.
Figure 1
Current practices of performing the Ask, Advise, and Assess, tobacco screening and counseling steps among PED/UC healthcare professionals
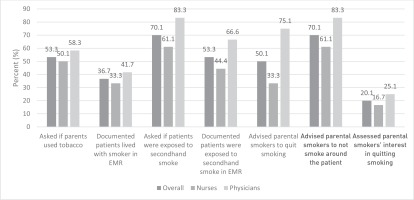
Figure 2
Current practices of performing the Assist and Arrange tobacco counseling steps among PED/UC healthcare professionals
Ask
Over half (53.3%) of participants reported they asked whether parents used tobacco, 36.7% documented that patients lived with a smoker in the EMR, 70.0% asked whether patients were exposed to secondhand smoke, and 53.3% documented the patients’ exposure status in the EMR (Figure 1).
Advise
Fifty percent of participants advised parental smokers to quit smoking, and 70.0% advised parental smokers not to smoke around patients (33.3% of nurses and 75.0% of physicians). Both professional groups had high percentages (70.0%) of advising parental smokers not to smoke around patients (61.1% of nurses and 83.3% of physicians) (Figure 1).
Assess
Only 20% of participants assessed parental smokers’ interest in quitting smoking (16.7% of nurses and 25.0% of physicians) (Figure 1).
Assist and arrange
Overall, only 16.7% of participants assisted/arranged parental smokers with smoking cessation efforts (Figure 2). Specifically, 16.7% of participants talked to parental smokers about smoking cessation techniques and tactics, 10.0% referred/enrolled parental smokers to the Tobacco Quitline or to a smoking cessation program, 6.7% made a quit plan with parental smokers, and 6.7% recommended NRT to parental smokers. No participants prescribed NRT to parental smokers.
Attitude and practice factors
Table 2 presents attitude and practice factors including levels of confidence, ease, effectiveness, optimism, and preparedness; level of importance; and barriers to tobacco counseling.
Table 2
Attitude and practice factors of tobacco counseling among PED/UC healthcare professionals
Level of confidence in tobacco counseling
Overall, 76.7% of participants were at least moderately confident in providing guidance on the harmful effects of parental smoking on children (Table 2). Participants reported they were at least moderately confident in: advising parental smokers to quit smoking and providing quitting materials to parental smokers (43.0%); assessing barriers to parental smokers quitting smoking (26.7%); assisting parental smokers by discussing smoking cessation techniques and tactics (23.3%); enrolling/referring parental smokers to the Tobacco Quitline (16.7%); and recommending (10.0%) or prescribing (3.3%) NRT to parental smokers.
Levels of ease, effectiveness, optimism, and preparedness in tobacco counseling
Overall, 57.5% of participants reported they were at least moderately optimistic that offering standardized efforts would reduce patients’ exposure, but only 36.7% found it at least moderately easy to identify secondhand smoke-exposed patients and counsel parental smokers (Table 2). Only 23.3% of participants perceived they were at least moderately effective in tobacco counseling, and 26.7% were at least moderately prepared to assist parental smokers to quit smoking.
Level of importance of tobacco counseling
Overall, most participants perceived the importance of intervening with tobacco users to improve patients’ health (86.7%), reduce future healthcare visits (70.0%), and to improve smokers’ health (76.7%) (Table 2).
Barriers to tobacco counseling
The top three barriers reported by both professional groups were: time limitations (93.3%), parental smokers’ lack of interest in being counseled (86.7%), and lack of professional training in the area of tobacco cessation counseling (80.0%) (Table 2).
Attitude and practice factors based on performing tobacco counseling
Table 3 presents attitude and practice factors based on performing tobacco counseling (the 5 As). Those who had higher levels of confidence, ease, effectiveness, optimism, and preparedness also had higher reports of engaging in the assess, and assist and arrange steps, while these factors varied among the ask and advise steps.
Table 3
Attitude and practice factors associated with performing tobacco counseling among PED/UC healthcare professionals
| Attitude and practice factors | The 5 As of tobacco counseling | |||||
|---|---|---|---|---|---|---|
| Asked whether parents used tobacco (n=16) | Asked whether patients were exposed to tobacco smoke (n=21) | Advised parental smokers to quit smoking (n=15) | Advised parental smokers not to smoke around patient (n=21) | Assessed parental smokers’ interest in quitting smoking (n=6) | Assisted/Arranged parental smokers (n=5) | |
| At least moderately confident in: | ||||||
| Providing guidance on the harmful effects of smoking on children | 14 (87.5) | 18 (85.7) | 13 (86.7) | 18 (85.7) | 6 (100.0) | 5 (100.0) |
| Advising parental smokers to stop smoking | 8 (50.0) | 9 (42.9) | 7 (46.7) | 10 (47.6) | 5 (83.3)* | 4 (80.0) |
| Assessing barriers to quitting | 4 (25.0) | 4 (19.0) | 4 (26.7) | 5 (23.8) | 4 (66.7)** | 3 (60.0)* |
| Assisting parental smokers by discussing smoking cessation | 5 (31.3) | 5 (23.8) | 4 (26.7) | 6 (28.6) | 4 (66.7)* | 4 (80.0)** |
| Providing quitting materials | 7 (43.8) | 8 (38.1) | 5 (33.3) | 8 (38.1) | 4 (66.7) | 4 (80.0) |
| Enrolling/referring to the Quitline | 4 (25.0) | 4 (19.0) | 3 (20.0) | 5 (23.8) | 3 (50.0)* | 2 (40.0) |
| Recommending NRT medications | 1 (6.3) | 1 (4.8) | 1 (6.7) | 2 (9.5) | 1 (16.7) | 1 (20.0) |
| Prescribing NRT medications | 1 (6.3) | 1 (4.8) | 1 (6.7) | 1 (4.8) | 1 (16.7)* | 1 (20.0)* |
| At least moderately: | ||||||
| Easy to identify patients exposed to tobacco smoke and to counsel parental smokers | 7 (43.8) | 9 (42.9) | 6 (40.0) | 10 (47.6) | 4 (66.7) | 3 (60.0) |
| Effective in identifying patients exposed to tobacco smoke and counseling parental smokers | 5 (31.3) | 5 (23.8) | 4 (26.7) | 6 (28.6) | 4 (66.7)** | 3 (60.0)* |
| Optimistic that offering standardized efforts to routinely identify patients exposed to secondhand smoke and counseling parental smokers will reduce patients’ exposure | 11 (68.8) | 14 (66.7) | 11 (73.3) | 14 (66.7) | 4 (66.7) | 3 (60.0) |
| Prepared to assist parental smokers to quit smoking | 7 (43.8)* | 7 (33.3) | 5 (33.3) | 7 (33.3) | 5 (83.3)*** | 44 (80.0)** |
| Tobacco counseling is important to: | ||||||
| Patients’ physical health | 15 (93.8) | 19 (90.5) | 13 (86.7) | 18 (85.7) | 6 (100.0) | 5 (100.0) |
| Patients’ future healthcare visits | 11 (68.8) | 15 (71.4) | 11 (73.3) | 14 (66.7) | 5 (83.3) | 4 (80.0) |
| Parental smokers’ physical health | 12 (75.0) | 16 (76.2) | 13 (86.7) | 17 (81.0) | 6 (100.0) | 5 (100.0) |
| Agree that barriers include: | ||||||
| Inadequate reimbursement for time it takes to counsel | 4 (25.0) | 6 (28.6) | 5 (33.3) | 6 (28.6) | 1 (16.7) | 1 (20.0) |
| Lack of professional training in the area of cessation counseling | 12 (75.0) | 16 (76.2) | 10 (66.7) | 16 (76.2) | 3 (50.0)* | 3 (60.0) |
| Time limitations | 14 (87.5) | 19 (90.5) | 14 (93.3) | 19 (90.5) | 6 (100.0) | 5 (100.0) |
| Parental smokers’ lack of interest in being counseled | 13 (81.3) | 17 (81.0) | 11 (73.3)* | 17 (81.0) | 4 (66.7) | 3 (60.0) |
| Parental smokers’ anger | 9 (56.3) | 13 (61.9) | 10 (66.7) | 12 (57.1) | 5 (83.3) | 3 (60.0) |
| Fear that counseling parental smokers is not effective | 8 (50.0) | 10 (47.6) | 7 (46.7) | 10 (47.6) | 3 (50.0) | 2 (40.0) |
| Lack of easily accessible information to give to parents | 11 (68.8) | 15 (71.4) | 9 (60.0) | 13 (61.9) | 3 (50.0) | 2 (40.0) |
| Hard to make systems level policy changes | 10 (62.5) | 13 (61.9) | 9 (60.0) | 12 (57.1) | 4 (66.7) | 3 (60.0) |
Chi-squared results indicated a larger proportion of participants who perceived themselves as least moderately prepared to assist parental smokers to quit smoking reported asking whether parents used tobacco (p=0.024). A lower proportion of participants who agreed that parental smokers’ lack of interest in being counseled was a barrier reported advising parental smokers to quit tobacco use (p=0.032). A higher proportion of participants who were at least moderately confident in advising parental smokers to stop smoking (p=0.027), assessing barriers to quitting (p=0.013), assisting parental smokers by discussing smoking cessation techniques and tactics (p=0.005), enrolling/ referring to the Quitline (p=0.014), or prescribing NRT (p=0.042), reported assessing parents’ interest in quitting smoking. Additionally, participants who reported effectiveness (p=0.005) and preparedness (p<0.001) had higher levels of assessing parents’ interest in quitting smoking. A significantly lower proportion of participants who agreed that lack of professional training in tobacco cessation counseling was a barrier, reported performing the assess step (p=0.040) (Table 3).
Similar to the assess step, a higher proportion of participants who were at least moderately confident in assessing barriers to quitting (p=0.003), assisting parental smokers by discussing smoking cessation techniques and tactics (p=0.034), or reported higher perceived effectiveness (p=0.034) and preparedness (p=0.003), reported higher levels of performing the assist and arrange steps (Table 3).
DISCUSSION
This study identified the current practices of tobacco screening and counseling among a sample of nurses and physicians who work at a high-volume, tertiary care children’s hospital PED/UC. Study results indicated areas of intervention development and will guide implementation of a tobacco cessation intervention for this setting aimed at reducing the high rates of child TSE among our population5. It has been long observed that US emergency care settings provide care for a large proportion of adult smokers23. The pediatric emergency care setting may represent an ideal opportunity to provide tobacco prevention and cessation education to pediatric patients and parental smokers who may not receive these efforts in other settings. PEDs/UCs are especially important because they serve as ‘safety nets’ for medically underserved populations who seek primary and specialty care in the emergency care setting24,25.
The present study revealed three key findings to inform intervention development efforts: 1) emphasizing the importance of providing tobacco counseling to parental smokers in the PED/UC setting to potentially improve pediatric patients’ health outcomes; 2) training PED/UC professionals on the Clinical Practice Guideline9; and 3) standardizing tobacco control efforts in the PED/UC setting.
Emphasizing the importance of providing tobacco counseling to parental smokers to improve pediatric patients’ health outcomes
Seventy percent of PED/UC professionals asked about patients’ TSE status and advised parental smokers not to smoke around their child, whereas only 50% of professionals asked about parents’ tobacco use and advised parental smokers to quit smoking. Notably, about 60% of nurses asked and advised about patients’ TSE, but only half asked about parents’ tobacco use, and one-third advised parental smokers to quit smoking. Further, over three-quarters of PED/UC professionals felt at least moderately confident in providing guidance on the harmful effects of smoking on children. Most PED/UC professionals deemed tobacco counseling to be important to patients’ clinical health and future visits. Although over three-quarters also found that tobacco counseling was important to parental smokers’ health, this percentage was lower than endorsements of importance to patients’ health and future healthcare utilization. Prior work at this PED/UC found that when compared with unexposed children, those who were exposed to tobacco smoke had significantly higher PED/UC resource utilization including diagnostic, radiologic, and laboratory testing and also a greater likelihood of being hospitalized13. Thus, if each PED/UC visit were used to initiate tobacco control efforts and provide brief counseling to parental smokers, the potential health benefits to both parents and their children could be substantial5,18. There may also be an associated cost benefit. A ranking of 28 evidence-based clinical preventive services based on cost-effectiveness and preventable burden found that counseling to prevent youth tobacco initiation, and adult tobacco use screening and smoking cessation efforts, were ranked second and third, respectively, after childhood immunizations26.
This study’s screening rates suggest there are currently missed opportunities to reduce PED/ UC patients’ TSE by intervening with their parents who smoke. Prior research among PED patients at this hospital found TSE prevalence of up to 48%5, which aligns with the TSE prevalence of 44% that PED/UC professionals estimated in this study. Up to 50% of parents and 30% of patients are not routinely asked about tobacco use and TSE. Additionally, only 37% and 53% of PED/UC professionals recently documented that patients lived with a smoker and were exposed to tobacco smoke, respectively. These findings align with a larger PED/UC study of EMR data that found 55% of patients did not have a documented TSE status15. While the proportion of professionals who performed the advise step was encouraging, only 20% progressed to the assess step. Not surprisingly, rates of performing the assist and arrange steps were even lower, with about 17% of professionals providing smoking cessation counseling, with only 10% enrolling/referring parental smokers to the Quitline or a smoking cessation program. These findings are similar to other studies among US pediatric nurses20 and pediatricians21. Of note, no healthcare professionals prescribed NRT medications to parental smokers, despite prior work indicating that two-thirds of parental smokers who bring their children to the present study’s PED/UC are interested in receiving NRT27. Cessation medications or behavioral counseling effectively increase abstinence among US smokers, and when used together, double the likelihood of successful abstinence11. However, less than one-third of US adult smokers use counseling or medications when making a quit attempt11. Thus, while it is important to offer brief behavioral counseling alone, PED/UC nurses and physicians should consider offering NRT medications to eligible parental smokers, even though they are not their direct patients. To develop an intervention that offers NRT to parents in our setting, we will train PED/UC professionals on how to assess contraindications to determine eligibility, and administer several weeks supply of NRT (e.g. nicotine patch, lozenges, gum) to interested parents.
Training PED/UC healthcare professionals on the Clinical Practice Guideline for treating tobacco use and dependence
Only one PED/UC healthcare professional reported receiving tobacco counseling training in the past 12 months, and only three were aware of the 5 As of tobacco counseling. Overall, 80% of PED/UC professionals agreed that lack of training was a barrier. Training was also a significant barrier identified to performing the assess step. Only a small percentage of PED/UC professionals felt at least moderately effective in or found it easy to identify tobacco smoke-exposed patients and counsel parental smokers. Only 27% felt at least moderately prepared to assist parental smokers to quit smoking. It is important to increase perceived effectiveness and preparedness, by training healthcare professionals on how to effectively identify exposed patients and counsel their parents on quitting smoking, and preparing them to assist parents with available referral resources (e.g. Tobacco Quitline). Studies of smoking cessation support delivered by nurses28 and physicians29 in any healthcare setting found that providing brief advice to patients is effective in promoting tobacco cessation and increasing quit rates. Encouragingly, we found a higher proportion of PED/UC nurses and physicians who actually performed the assess, and assist and arrange steps, in the past 30 days, perceived themselves as at least moderately: effective in identifying tobacco smoke-exposed patients and counseling parental smokers, prepared to assist parents to quit smoking, and confident in performing the advise, assess, and assist and arrange steps. Taken together, our findings highlight the importance of increasing confidence, preparedness, and effectiveness of providing tobacco counseling during training. Based on the present study’s findings, one potential consideration is to identify a PED/UC healthcare professional to serve as a ‘super trainer’ during intervention delivery. This professional could potentially be trained as a Tobacco Treatment Specialist, and in turn, could help train other healthcare professionals and answer any questions on an ongoing basis.
Other barriers identified by PED/UC professionals were time limitations, parents’ lack of interest in being counseled on tobacco, lack of easily accessible information, and parent anger. These findings parallel other research indicating the majority of pediatric nurses endorsed parent resistance to cessation discussions (89%) and lack of training (57%) as barriers20. Not surprisingly, the barrier of parents’ lack of interest in being counseled was associated with lower rates of advising parents to quit smoking. Providing education to PED/UC nurses and physicians could reduce these barriers by providing information on the effectiveness of brief interventions (e.g. <3–5 minutes9) and how to deliver tobacco cessation interventions in a non-threatening way. While limited time was the most endorsed barrier, the long wait times in the PED/ UC setting may allow for the implementation of interventions without disrupting clinical flow30,31. For example, 60% of US patients who present to an ED have to wait at least 15 minutes to see an advanced practice registered nurse, physician, or physician assistant3.
Standardizing tobacco control efforts in the PED/UC setting
Our findings support the need to standardize tobacco control efforts for emergency clinical practice. Nearly two-thirds of PED/UC healthcare professionals did not have a standardized, routine system for screening patients for TSE, yet 90% endorsed the need for such a system. A universal screening and counseling system might also mitigate concerns that parents would feel angry or ‘singled out’. This type of system would facilitate the identification of those who want to quit. Annually, about 70% of US adult smokers want to quit, but only 50% make a quit attempt11. Thus, having standardized screening and counseling systems in place would identify those who are willing to quit and provide resources to use after their child’s PED/UC visit. For example, a universal question could be routinely asked about patients’ TSE status during the same timepoint of each clinical encounter by an appointed healthcare professional (e.g. during triage by a nurse). Those who screen ‘positive’ for child TSE could be followed up during their visit with an EMR prompt to remind healthcare professionals to provide parents with TSE reduction and tobacco cessation education and helpful resources (e.g. before discharge by the bedside nurse). Emphasizing the potential associated positive child health outcomes (e.g. improvements in patients' overall health status) might increase implementation of these initiatives.
Limitations
This study was conducted with a small sample of PED/UC healthcare professionals from a single US children’s hospital, and results may not be generalizable to other emergency settings. We recruited 30 participants to pilot the survey tailored to the PED/UC population, which was derived from existing instruments disseminated at the national level among members of national organizations (i.e. AAP and Society of Pediatric Nurses) 20,21. The current study was the first step in a study to develop and test a comprehensive tobacco treatment program at this hospital. Our results align with studies of pediatric healthcare providers, which also reported similar barriers to conducting tobacco screening and counseling14,32. Additionally, our study had low representation of racial/ethnic minorities. Further, the current study’s PED is part of the Pediatric Emergency Care Applied Research Network (PECARN) that includes other US PEDs, which provide care for similar patient volumes and relatively similar populations33. Our results are informative to the current PED/UC for intervention development and may also inform development efforts in similar settings. However, more research is needed and future research should include a larger surveillance study administered to nurses and physicians employed at PEDs/UCs nationwide. Moreover, we collected self-reported data, and did not conduct observations of tobacco counseling-related behaviors during PED/UC visits. It is possible that underreporting or overreporting of these practices may have occurred. This study was conducted at one timepoint, and causal relationships cannot be drawn. This study intentionally focused on patients’ exposure to secondhand smoke from combustible tobacco products (e.g. conventional cigarettes) and not exposure to secondhand aerosol from e-cigarettes as this parent population has very low e-cigarette use rates (<5%)34. Several independent comparisons were conducted to assess the bivariate relationships between PED/UC professionals’ perceptions and tobacco use counseling behaviors performed. Due to the small sample size, we did not assess these relationships by professional group, and multiple comparisons were not adjusted for in each test due to the potential for identifying false negatives.
CONCLUSIONS
Results of this study’s survey of PED/UC nurses and physicians indicate there is a need to increase current tobacco counseling behaviors. Professional training in this area is highly warranted to increase levels of confidence, effectiveness, and preparedness in addressing child TSE and parental smoking among nurses and physicians. Related policy and practice strategies to standardize these pediatric tobacco control efforts should also be considered at the current hospital. Future research is needed to adapt and implement the Clinical Practice Guideline for use within the PED/UC clinical flow.


