INTRODUCTION
More than 4 million visits to emergency departments (EDs) annually involve treatment of children with complaints that are potentially related to tobacco smoke exposure (TSE)1. Over 30% of children who visit the pediatric ED (PED) for TSE-related illnesses live with parents who smoke2,3. The economic costs attributable to lost productivity due to smoking and TSE are estimated to be $190.7 billion and $7.2 billion, respectively. Counseling- and pharmacologically-based cessation interventions are cost-effective4,5 but the costs of PED-based cessation interventions are unknown.
We conducted the ‘Healthy Families’ study, an IRB-approved randomized controlled trial (RCT) of 750 parents that smoke and who presented with their child with a potential TSE-related illness to the PED or Urgent Care (UC) unit of a Midwestern Children’s Hospital. The goal of this RCT was to evaluate the efficacy of a screening, brief intervention, and assisted referral to treatment (SBIRT) condition to help parents quit smoking (n=377) compared with an attention control condition6.
We examined the costs associated with implementing the program so that planning, staffing and resource allocation can be provided for future cessation interventions. Herein, we report all associated costs from the organizational perspective (that of the providing hospital), including interventionist training, screening and enrollment, and SBIRT delivery.
METHODS
Following standard procedures7,8, we documented costs (in 2018 US$) associated with replicating the interventions in non-research settings, excluding development/evaluation costs. We used micro-costing9 rather than gross-costing techniques, identifying costs for each intervention element. No overhead costs are reported, as all activities are anticipated to be conducted by regular staff members with only minimal impact on their overhead needs.
One objective of this RCT was to ensure that many staff members gained experience with SBIRT delivery. Thus, some costs would not accurately represent the typical experience of a PED delivering the SBIRT. Here we report costs incurred if the RCT had been conducted to ensure adequate coverage while optimizing efficiency. The resulting scenario would have one supervisor (a tobacco treatment director, TTD) and two tobacco treatment interventionists (TTIs) with responsibilities totaling around 30 hours/month during which 20 parents who smoke, per month, are given the SBIRT. These roles would typically be assumed by social workers or PED staff (e.g. research coordinators).
Sensitivity analyses included the effects of higher and lower: interventionist salaries, number of treated parents, intervention delivery length; and a scenario in which the ED belongs to a smaller general acute care hospital with lower rates of social worker turnover. An Excel spreadsheet is provided (Supplementary file) so organizations can enter their own cost assumptions.
RESULTS
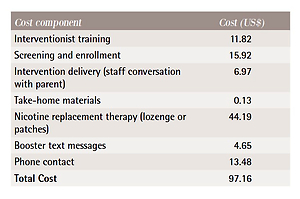
The mean (SD) age of smokers was 31.8 (7.7) years; the majority were female (86.8%), Black (52.7%), had public or no insurance (87.3%), and had an income level of ≤$15000 (64.6%). The median (IQR) number of daily cigarettes was 10 (6–15). Table 1 displays the total mean US$ cost per treated parent, using the assumptions associated with providing the SBIRT on a scale comparable to our hospital.
Table 1
Total mean cost per treated parent, main analysis
During the RCT, mean enrollment was 19.8 parents per month (range: 5–42). To treat ≤42 parents per month, three staff members were deemed sufficient: the TTD and two TTIs. Based on our hospital’s labor costs, we assume the TTD is paid $28.74/hour plus 26% for benefits and statutory wage-based expenses totaling $36.21/hour. The TTIs are paid $19.30/hour plus the 26%, totaling $24.32. For sensitivity analyses, we use the upper and lower ends of the salary scale for these positions at our hospital, and for the benefits plus statutory expenses, we use the FY2017 rate of 25.5% (low end) and the FY2019 rate of 26.5% (upper end).
For all intervention activities (excluding training), the main analysis assumes that the TTD treats 6 and the TTIs treat 7 out of 20 families in an average month. The average labor cost is thus $27.88/hour. All interventionists receive three types of SBIRT-related training.
Motivational interviewing (MI) training
To minimize expenses, we assume the TTD and TTIs will complete their training online (e.g. AAP program, https://shop.aap.org/eqipp-treating-tobacco-product-use-and-exposure-in-families/) for $199, plus six hours to complete the program.
Tobacco treatment specialist (TTS) training
Here, we include costs for the self-paced, BREATHE Online program10 (27 hours plus exam at $800). After completing 240 hours of field work, the TTS can receive certification for $150 to become a Certified TTS. For the cost analysis, we include the value of 27 hours at the staff member’s payment rate plus $950, not the value of the 240 hours of field work.
Assisted referral training
The TTIs are trained in delivering brief smoking cessation and TSE reduction counseling and direct connection to the Quitline, SmokefreeTXT program, or smokefree.gov. We account for 3 hours of training beyond the original TTD: two hours by the TTD and a 1-hour refresher. Further, we include 3 hours for the TTD to plan referral options and develop their training and other intervention protocols. Intervention fidelity is assured by having the TTD listen to ten 30-minute audiotapes for each TTI, which will inform the assisted referral refresher.
For each staff member, their training costs are divided by the number of families they would be expected to work with over the course of their tenure with the providing organization. We estimate 5 years per TTD and 2 years per TTI. Total training costs would thus be $2453 for a TTD, or $6.81 per parent treated by the TTD, and $2314 for a TTI, or $13.77 per parent treated by the TTI. Using the assumption that 30% of parents are treated by the TTD, average training costs are thus $11.69 per treated parent.
In the RCT, parents were screened by staff using our hospital’s electronic medical record system. The TTD and TTIs identified potential parents; 5145 parents were approached and the staff member spent an average of 5 minutes to determine interest and eligibility, averaging approximately 11 hours/month. The enrollment cost was $15.92 per treated parent.
The SBIRT is delivered while the child is in the PED/UC. The staff member screens for nicotine replacement therapy (NRT) contraindications and gives instructions on NRT use. They deliver the SBIRT and facilitate access to cessation resources (e.g. Quitline). The average SBIRT time was 15 minutes (range: 5–35 minutes); reasonable low and high scenarios are 10 and 20 minutes, and we also examined the effects of 30 minutes. For the average family, the cost was $6.97, while for 30 minutes the cost would be $13.94.
All interested and eligible parents received a 6-week supply of NRT, with their choice of lozenge ($69.75) or patch ($65.34). Of the 384 SBIRT parents, 129 chose patches and 70 chose lozenges at baseline. During follow-up phone calls, 50 chose to receive an additional six weeks of NRT: 30 chose patches. Average spending was $43.40 per enrolled parent.
Each parent received a packet of free take-home materials; associated costs are envelopes ($12.99 for a box of 100; $0.13 per family). After the SBIRT, staff set up weekly booster text messages for 12 weeks; estimated time was 10 minutes per parent, averaging $4.65.
All parents are contacted by phone to complete assessments to determine their smoking behavior, their child’s TSE patterns, and if they had quit smoking. In a non-research related scenario, supportive topics would be included such as help with quit attempts and managing relapses. All parents were required to complete a phone call; an estimated average of 20 attempts are necessary. We estimate 1 minute and 10 minutes for each unsuccessful and successful call, respectively, or 29 minutes per parent, costing $13.48. This time would also be appropriate to offer supplemental NRT. For the RCT, this was offered during a home visit, not included in the cost inventory as it was used for research activities.
We conducted sensitivity analyses in which using the lower salary rates yields a cost per parent of $85.42, and with the higher rates, the cost is $108.99. For 30 or 10 parents per month, the cost per parent is $87.70 or $124.26, respectively.
For the general acute care hospital scenario, the new assumptions were: a) 300 Medicaid pediatric patients visit the ED annually with a potential TSErelated diagnoses, of which 35% have a parent who smokes, b) non-Medicaid patients with similar diagnoses are assumed not to have non-smoking parents, and c) interventionists are two social workers who are long-term employees, paid at the higher (TTD) salary level from the main analysis, and both are trusted to maintain intervention fidelity, so no audiotape reviews are needed. The average cost per treated parent (3.75 parents per month) would be $98.60, similar to $97.16 from the main analysis.
DISCUSSION
This study describes the costs of implementing an SBIRT intervention for parents who smoke visiting the PED/UC with their child. It also provides a tool that EDs/UCs can use to estimate the costs of providing this service to parents who are smokers, including interventionist training, parent enrollment, and the intervention itself. ED/UC visits represent an important teachable moment for parents on smoking cessation11. Specific to PED-based cost analyses, a PED study found that offering an influenza vaccine to all eligible children was cost-effective compared to other strategies, and had the lowest cost of $114.45 per influenza case prevented12. Specific to substance use, ED-initiated brief intervention with medication treatment for opioid dependence had high value and was likely more cost-effective than a brief intervention and referral to community-based treatment or referral only13. Therefore, providing preventive interventions in the ED may be a generally cost-effective strategy.
The accompanying spreadsheet tool will allow for organizations to estimate their own US$ costs for each aspect of the intervention. Some of the cost components could differ among organizations. For example, many social workers will have already received training in MI. Additionally, a TTS core competency for evidence-based tobacco use treatment is the demonstration of effective MIbased counseling skills to promote behavior change to individuals with a tobacco use disorder14. For example, the BREATHE TTS course focuses solely on counseling skills for nearly 20% of the program10.
Parent screening costs could be reduced by advertising the SBIRT counseling as a service parents could request. Hospitals could either decide not to provide NRT or offer it to all eligible parents who smoke. In our RCT, parents were interested in receiving free NRT, the majority reported using NRT and half requested an additional supply15. A Cochrane review reports that use of NRT increases quit rates by 50%–60%, irrespective of treatment setting16. Prior studies have deemed NRT to be cost-effective and comparably inexpensive to other medical services17. For example, a study that compared physician advice and NRT use compared to physician advice-only found that NRT resulted in one additional lifetime tobacco quitter with a cost of about $730018. Additionally, the use of NRT has been reported as cost-effective for preventing smoking relapse among recently abstinent smokers and those attempting to quit 19.However, the U.S. Surgeon General’s Report indicates that in the clinical setting, 66.6% of adult patients are screened for tobacco use and, of those, 20.1% receive counseling and only 3.8% receive a prescription for cessation medication including NRT5. This report indicates about 3 in 10 adult tobacco users used medication (29.0%) or used counseling with medication (31.2%), which is encouraging. Thus, including NRT as an ongoing component in a future similar trial is highly warranted.
Limitations
There are limitations to be considered. The study reports only costs from the organizational perspective, that of the providing hospital. From the societal perspective, costs incurred by the participating parents (e.g. opportunity costs of their time, quit attempt expenses) should also be included. Also, we were not able to use the cost data in a cost-effectiveness analysis since the RCT did not obtain differences in cessation outcomes20. Higher quit rates may have been observed if the service was advertised, with interested parents seeking it out and then a cost-effectiveness analysis could have been conducted to demonstrate the value of the SBIRT.
CONCLUSIONS
PED/UC visits for TSE-related illnesses present opportunities for SBIRT interventions with parents who are smokers. The cost data provided should be generalizable to a variety of adult tobacco users that seek care in the adult or PED/UC setting. Since the emergency setting is an important locus of tobacco control that could have a large public health benefit, every emergency visit should be used to provide cessation counseling21. Thus, findings from this study can be used for planning and implementation of tobacco cessation interventions into emergency visits.