INTRODUCTION
Smoking cessation is challenging but can be achieved through community and individual-level interventions1. While high income countries have successfully adopted both forms of interventions to reduce their burden of smoking, low- and middle-income countries (LMICs) have lagged in the adoption of individual-level interventions2,3. In India, although national public health policies have marginally improved cessation rates, individual-level smoking cessation, community health worker, text messages, mobile health, lowand-middle-income country smoking cessation counseling remains inadequate4,5. Smoking cessation support, delivered through readily available modes of communication and tailored to an individual’s readiness to quit, can potentially increase smoking cessation rates in LMICs such as India.
Traditionally, community health workers (CHWs) in India have served as a bridge between patients and healthcare resources for the management of communicable, maternal, and newborn diseases6,7. In 2013, the government of India expanded the role of CHWs to promote healthy lifestyle habits such as smoking cessation, through community and home-based counseling sessions8. However, inadequate training, support, and the inherent difficulty in achieving behavior change have led to most CHWs feeling underprepared and overburdened, warranting additional external support9. Mobile health solutions in the form of text messages have been shown to be effective in promoting smoking cessation across a wide range of age groups and could potentially provide external support to enhance CHW efforts10,11. In 2015, the government-initiated Cessation program established a nationwide mobile health intervention that provides smoking cessation support via text messages to those willing to quit12. Although nearly 2 million individuals have registered for the program, most feel the need for additional in-person smoking cessation counseling as a supplement to the program’s efforts13. A multi-component intervention combining CHW and text messaging-based interventions could potentially have a synergistic effect in increasing smoking cessation rates.
Motivational interviewing (MI) is a patient-centered style of communication that has been shown to improve smoking cessation rates among those who have a low desire to quit and resist participation in cessation programs14,15. Additionally, MI has been effective in promoting smoking cessation across a wide range of age groups16. Although mostly used in high income countries by trained smoking cessation counsellors17, its use by lay health workers in LMICs has recently been shown to be promising18. Despite its effectiveness in improving smoking cessation rates, MI has previously not been evaluated for delivery by CHWs in India.
While the combined use of CHWs and text messaging can potentially improve smoking cessation rates, there is no evidence to prove its effectiveness in LMICs. To fill this gap in evidence, we tested a Multi-Unit Kit for Tobacco cessation in India (MUKTI), incorporating CHW-led home visits and mobile text messages, tailored to an individual’s readiness to quit, and hypothesized that such an intervention would result in higher cessation rates compared to brief education alone.
METHODS
Study setting and population
A detailed description of the study design has been previously given19. Briefly, between April 2018 and August 2019, we conducted a mixed methods two arm, parallel, pragmatic, cluster randomized controlled trial with qualitative analysis at the end of intervention in a semi-urban town, Dalkhola, West Bengal, India. The town has a population of about 20000 people with an estimated prevalence of smoking of 14% among adults20,21. Using the voter list as a reference, the town was divided into geographical clusters consisting of equal population sizes. One female CHW was assigned to each geographical cluster who screened, enrolled, and later delivered the intervention.
We included all adult participants (aged 18–70 years) who self-reported their current daily use of cigarettes or bidis (hand rolled tobacco leaves) and had access to a mobile phone that had the capability to send and receive text messages. Bidis have a higher nicotine concentration (21 mg/g vs 13 mg/g) compared to conventional unfiltered cigarettes and are cheaper than cigarettes22. Participants who were bed-bound for any acute or chronic condition, had a significant disability such as being blind, deaf or intellectually disabled, preventing them from meaningfully participating in the trial were excluded from the study. Furthermore, the CHW had discretionary power to exclude any eligible participant based on her assessment of their ability to participate effectively in the trial and follow-up at the end of the intervention period.
Study design and intervention
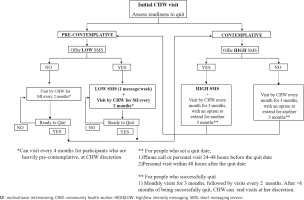
The content and dose of the intervention were tailored to an individual’s readiness to quit, determined using the trans-theoretical model of behavior change23. Based on the response to the question ‘Are you ready to quit in the next 6 months?’ at the beginning of the study, eligible participants were categorized into being pre-contemplative or contemplative to quitting smoking. The two main components of the intervention included CHW-led home-based smoking cessation counseling and culturally appropriate text messages delivered through mobile phones (Supplementary file Table 1). MI techniques were used by CHWs visiting participants who were pre-contemplative to the idea of smoking cessation.
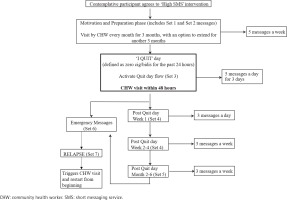
CHWs in the study are individuals from the local community who are carefully selected through a written test and interview process and trained to provide smoking cessation counseling24. Once selected, each CHW underwent a one-week didactic session coupled with interactive role-playing to teach them MI techniques of communication. Additionally, each CHW had access to a detailed training booklet and a flipbook containing smoking cessation counseling material. The text messages were derived from a databank of messages that were previously used in a large smoking cessation clinical trial conducted in Australia25. Each of these messages were modified to make them culturally acceptable and translated into two local languages, Hindi and Bengali. The messages were then grouped into different sets, each targeting participants at different trans-theoretical stages of change (pre-contemplation, contemplation, determination, action, relapse, maintenance) and were automatically delivered to participants through a pre-defined algorithm. The algorithm was developed and customized using the open source software RapidPro26. Each delivery algorithm was activated by the user using a pre-defined code word, designated to their trans-theoretical stage of change. However, beyond activation of message sets using pre-defined code words, there was no further two-way communication or text message customization.
The intervention followed a dynamic process in which each participant had the ability to transition from one section of the intervention to the other based on their trans-theoretical stage of change, assessed by the CHW at every scheduled home visit. All participants received CHW-led home visits at varying frequencies but the mobile health component was optional. Pre-contemplative participants received a CHW home visit every 2 months and 1 text message every week describing the benefits of smoking cessation. Contemplative participants received a CHW visit once a month for 3 months and were asked to set a quit date. The CHW visits and text messages focused on motivating and preparing the participant to quit smoking. After the quit date, the intervention was focused on avoiding relapse. Participants who relapsed received a CHW visit that focused on identifying potential reasons for relapse and reassessed their readiness to quit (Figures 1 and 2).
The MI sessions were unscripted and CHWs used various methods (open-ended questions, repeating back information, showing empathy and summarizing) of MI27. CHWs encouraged patient engagement in the conversation by developing a discrepancy between the patient’s goals (such as health) and current behavior of smoking (building inner conflict). In addition, they explored ambivalence regarding smoking cessation, while avoiding argument or judgement. If participants expressed an interest in quitting, CHW visit and text message frequency were increased according to the contemplative workflow of the intervention.
Given that access to nicotine replacement therapy (NRT) was not widely available at the access site, it was made accessible through the CHW at market prices. At trial initiation, all control group participants received brief education through a single CHW-led home visit regarding the benefits of smoking cessation. All outcomes were measured at the end of 12 months after the start of the intervention. The primary outcome of interest was 14-day self-reported abstinence, biochemically verified by measuring exhaled carbon monoxide (CO) levels. The use of exhaled CO is a commonly used metric that is easily obtained, but less accurate when compared to measurement of blood levels of nicotine metabolites28. A validated breath analyzer was used by the CHW to measure CO levels at the end of the intervention period and a cut-off point of <10 parts per million was used to confirm smoking cessation29. Secondary outcomes included variation in quit rates based on participant age and education status. At the end of the intervention, a sample of CHWs and participants were interviewed to understand their perspectives on the intervention. A semi-structured guide was used to facilitate an open discussion during the one-on-one phone interview conducted by one of the investigators (AK), a physician who is a native of the town, in the interviewee’s local language. All discussions were audio-recorded and subsequently translated into the English language. Thematic analysis was conducted by two of the investigators (VH and AK) who evaluated all the CHW and participant interview transcripts independently, to identify common prevailing themes.
Prior to participation, all eligible participants were required to provide written informed consent. The institutional review board of University Hospitals Cleveland Medical Center in the USA and Society for the Promotion of Ethical Clinical Trials (SPECT), an independent review board in India, provided approval for this study. The trial was registered in the clinicaltrials.gov database (NCT03495622).
Statistical analysis
Sample size calculation for this study was based on the clustered pattern of delivering the intervention. It was calculated using a two-way significance level of 0.05, a power of 80%, minimum detection rate of 3.9% and an intra-class CI of 0.04. An attrition rate of 30% was anticipated and the final estimated sample size was 560 participants, 35 per cluster across 16 clusters and two sites. Although the initial study protocol was designed to test the intervention at two sites, numerous site-level barriers to implementation led us to confine the study to a single site. Here, we report results from the single site, Dalkhola, which consisted of 8 clusters, 5 for intervention and 3 for control. Using an intention-to-treat analysis format, the Pearson’s chi-squared test was used to compare the unadjusted and hierarchical logistic regression accounting for clustering at sites to compare adjusted cessation rates. Furthermore, we estimated all a priori secondary outcomes using similar regression tests and examined the cluster-level variability in uptake of the intervention and cessation rates. As sensitivity analysis, we compared cessation rates between groups in an as-treated format, among those who received an optimal dose of the intervention, defined as receiving ≥3 CHW-led home visits plus ≥5 text messages. The analysis was performed using the R software v3.5.2.
RESULTS
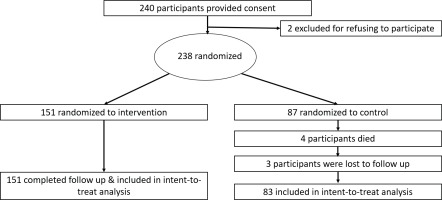
Among 240 eligible participants, a total of 238 participants (mean age 43±12.3 years; 96.2% male), 151 in the intervention group and 87 in the control group, provided informed consent. Half of the study cohort smoked bidis only and nearly 20% of the population smoked both cigarettes and bidis. At baseline, the majority of the participants had made no prior quit attempt and were predominantly (84.6%) pre-contemplative to the idea of smoking cessation (Table 1). At the end of 12 months, a total of 4 participants in the control group died and 3 participants were lost to follow-up resulting in an overall retention rate of 97%. The participants who died were excluded and those who were lost to follow-up were considered to be smokers at the end of the study period (Figure 3)28. With regard to the primary outcome, a total of 31 (20.5%) participants in the intervention group and 9 (10.8%) in the control group quit smoking with an absolute difference in cessation rate of 9.7% (RR=1.69; 95% CI: 0.04–71.33, p=0.74) (Table 2).
Table 1
Baseline participant characteristics
| Characteristics | All (N=238) n (%) | MUKTI (Intervention) (N=151) n (%) | Brief advice (Control) (N=87) n (%) |
|---|---|---|---|
| Sociodemographic | |||
| Age (years), Mean (SD) | 43.0 (12.3) | 41.8 (12.0) | 43.0 (12.2) |
| Male | 225 (96.2) | 147 (97.3) | 82 (94.2) |
| Religion | |||
| Hindu | 222 (93.3) | 142 (94.0) | 80 (91.9) |
| Muslim | 12 (5.0) | 5 (3.3) | 7 (8.0) |
| Other | 4 (1.7) | 4 (2.6) | 0 |
| Education level (school years), Mean (SD) | 9.31 (3.77) | 9.48 (3.7) | 9.30 (3.7) |
| Work status | |||
| Gov. employee | 14 (6.0) | 11 (7.2) | 3 (3.4) |
| Private employee | 48 (20.4) | 26 (17.2) | 22 (25.2) |
| Self-employed | 95 (40.4) | 91 (60.2) | 5 (5.7) |
| Unemployed (able to work) | 39 (16.6) | 9 (5.9) | 30 (34.4) |
| Unemployed (unable to work) | 13 (5.5) | 3 (1.9) | 10 (11.4) |
| Refused to answer | 16 (6.8) | 4 (2.6) | 12 (13.7) |
| Other | 10 (4.2) | 5 (3.3) | 5 (5.7) |
| Comorbidities | |||
| Prior history of respiratory disease | 7 (3.0) | 6 (3.9) | 1 (1.1) |
| Prior history of heart attack | 3 (1.3) | 2 (1.3) | 1 (1.1) |
| Prior history of stroke | 3 (1.3) | 3 (1.9) | 0 |
| Smoking related information | |||
| Cigarettes/day*, Mean (SD) | 4.02 (2.28) | 4.32 (2.48) | 3.67 (2.29) |
| Bidis/day**, Mean (SD) | 8.60 (4.63) | 9.00 (4.93) | 7.91 (4.63) |
| Smoke cigarettes only | 65 (27.3) | 34 (22.5) | 31 (35.6) |
| Smoke bidis only | 119 (50.0) | 76 (50.3) | 43 (49.4) |
| Smoke cigarettes and bidis | 43 (18.0) | 30 (19.8) | 13 (14.9) |
| Use pipe tobacco | 1 (0.4) | 1 (0.6) | 0 |
| Prior quit attempt | 9 (5.7) | 8 (5.2) | 1 (1.1) |
| Contemplative stage of behavior change | 23 (15.4) | 21 (13.9) | 2 (2.2) |
Table 2
Smoking cessation rates by intervention (MUKTI) and control
Figure 4
Cluster-level variability in intervention uptake and smoking cessation rates (data for 5 intervention clusters)
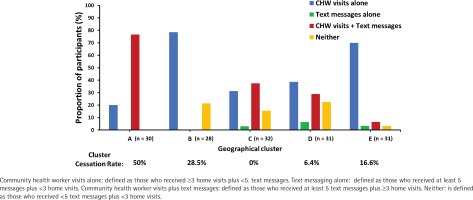
Secondary outcomes examining quit rates based on participant age and education level are shown in Table 2. Participants aged ≤40 years and those with ≥10 years of schooling demonstrated greater smoking cessation rates compared to older and less educated individuals, however, the difference was not statistically significant. Furthermore, there was large cluster-level variation in the overall uptake of an optimal dose of the intervention (0–76.6%) and cessation rates (0–50%; Figure 1) with an intra-class CI of 0.05. There was negligible uptake of NRT, with only one participant obtaining NRT from the CHW.
In the as-treated analysis, uptake of the intervention was examined by estimating the proportion of participants who received an optimal dose of the intervention, defined as ≥3 CHW visits and ≥5 text messages. A total of 46 (30.4%) participants received an optimal dose of the combined intervention. Among these participants, 17 (36.9%) quit smoking with an absolute difference in cessation rate of 26.2% (RR=4.58; 95% CI: 0.11–191.29, p=0.37) (Table 2).
For the qualitative interviews, 3 (60%) CHWs – each achieving different cluster-level cessation rates (0–50%), were chosen. All CHWs were female and had equal prior experience with home-based smoking cessation counseling. A total of 4 (3%) male participants (mean age 27.2 ± 2.5 years; average 10 cigarettes/day) in the intervention arm volunteered to participate in an interview. Two of these participants had quit smoking by the end of the study, and only one had received an optimal dose of the intervention (both components at high doses). The important prevailing themes identified during the CHW and participant interviews are detailed in Table 3.
Table 3
Community health worker and participant perspectives
DISCUSSION
In this mixed methods cluster randomized controlled trial, we evaluated the effectiveness of a multi-component smoking cessation intervention involving CHW-led home-based counseling and text messages, tailored to an individual’s readiness to quit. At the end of the study period, a greater number of participants in the intervention arm quit smoking compared to those in the control arm. However, the difference between the groups was not statistically significant, most likely due to low statistical power. Younger participants and those with 10 or more years of schooling had greater rates of smoking cessation. The potential impact of comorbidities on our outcomes is uncertain as only 13 (5.5%) participants reported to have comorbidities. Marked cluster-level heterogeneity in the uptake of intervention components and smoking cessation rates were noticed. Additionally, within an as-treated analysis, a positive dose-response relationship was noticed among those who used both components of the intervention.
The relatively large proportion (37%) of participants who quit smoking after receiving an optimal dose of the combined intervention suggests that a greater amount of support provided through CHW and text messages may be an effective solution to improve smoking cessation rates in India. However, the potential effectiveness of this finding is limited by the willingness of participants to receive the intervention at high doses. Only 30% of participants in the intervention group received an optimal dose of the intervention. The large cluster-level variability in uptake of the intervention is most likely a reflection of the varying ability of CHWs to engage participants. Furthermore, our results demonstrate that younger and more educated participants have higher smoking cessation rates – a finding consistent with other reports30,31. These observations can be explained by the fact that young, educated participants are high users of their mobile phones and may respond better to CHW-led counseling efforts. The cessation rate of 10.8% in the control group is greater than the national average of 5% reported in 2015 – an unexpected finding4. The higher quit rates could reflect underlying secular trends due to the effect of national public health policies which have raised the cost of cigarettes and bidis, introduced graphic warnings on tobacco products and conducted mass media campaigns to promote smoking cessation32. Notably, qualitative interviews at the end of the trial demonstrated that CHW-led smoking cessation interventions are not only feasible but also a preferable mode of counseling. The home-based CHW model can improve access to individual-level counseling in low-and-middle-income countries such as India and facilitate additional support from family members.
Despite the government-led implementation of separate CHW and mobile-based smoking cessation interventions, there is limited evidence to support the effectiveness of either intervention in India, especially in the context of tailoring the intervention based on an individual’s readiness to quit. A study evaluating the effectiveness of a single session of home-based CHW-led cessation counseling, combined with training in vedic exercises, resulted in a 2% absolute increase in cessation rates in the intervention group over a follow-up period of 6 months33. Similarly, in a prospective evaluation of individuals enrolled in the text messages-based mCessation program in India, 77% of participants reported that the messages are extremely helpful to quit smoking, and 19% of participants quit 6 months after enrollment13. However, this analysis is limited by the lack of a control group and the self-reported assessment of smoking cessation status. To the best of our knowledge, ours is the first study to evaluate a combined CHW and text messaging-based intervention, substantially adding to the existing body of evidence. Although the difference between our two study arms was not statistically significant, a cessation rate of nearly 20% over one year in the intervention arm is similar to estimates from other national and international smoking cessation trials10,11.
Our study has several advantages. First, multiple theory-based smoking cessation interventions have primarily focused on tailoring the content of the intervention to an individual’s readiness to quit (Web or mobile-based text messages)34,35. By tailoring the dose and content of our intervention components, we were able to focus a higher dose of the intervention towards those who were willing to quit and simultaneously use evidence-based MI techniques to motivate those who were not. Such a strategy can potentially reduce CHW burden. Additionally, while most similar studies often exclude those who are not motivated to quit, we demonstrate that the CHW-led model of motivational interviewing can be a potential solution to motivate individuals in quitting smoking. Second, the pragmatic study design made the text messaging component optional to the user and facilitated the dynamic transition of participants from one trans-theoretical stage of change to the other throughout the study period. The poor uptake of the mobile-based smoking cessation intervention in our study highlights the existing challenges of a mobile-based intervention in India, which has previously been shown to be ameliorated by promotion of text messaging based smoking cessation services by physicians36. Technology is continuously evolving and at the time of study inception, text messaging was the most commonly used mode of communication. However, the potential financial burden of receiving text messages and text messaging fatigue are some of the reasons cited by participants who opted out of the mobile-based component of the intervention. Given their widespread use and ability to send or receive picture and text messages at zero additional cost, multimedia messaging applications such as WhatsApp may be a preferred choice for future mobile health solutions in LMICs37. Third, this study highlights the feasibility of training lay CHWs in the use of MI techniques, a proven form of smoking cessation counseling in a clinic setting. A review of studies incorporating MI techniques to counsel smokers, demonstrated an overall weighted cessation rate of 17%, similar to rates within our study cohort17. Fourth, this study demonstrates the acceptability of home-based CHW-led smoking cessation counseling in a semi-urban region of India. Due to the lack of adequate healthcare facilities in the region, such non-physician led interventions can be a sustainable and cost-effective solution to the large burden of smoking-related diseases. CHW-led counseling is particularly appealing as CHWs have the ability to spend adequate amount of time with the participant, provide intervention within the participant’s home, and are able to involve family members who may be able to assist in achieving sustainable smoking cessation38. Finally, our qualitative interviews highlight the gaps and opportunities in combined smoking cessation interventions, which require further evaluation with multimedia mobile applications and larger sample sizes. Future interventions should focus on improving CHW training to enhance participant engagement, use multimedia applications instead of regular text messaging, and incorporate real-time data analysis to detect inadequate engagement and provide CHW supportive feedback.
Limitations
These results are to be interpreted in the context of several limitations. First, although our study protocol was designed to accommodate two sites within India, we were unable to implement our intervention at the second site in Jabalpur, India. This led to a lower than estimated sample size. Second, uptake of the intervention varied across clusters with many not receiving an optimal dose of the combined intervention. This was a consequence of the pragmatic study design, where text messaging was made optional to the participants. However, the positive dose-response relationship noticed in this trial highlights the potential benefits of combining these interventions and serves as a proof of concept for future clinical trials. Third, while all the CHWs were female, the majority of our study population was male, which may have influenced our study findings. Future studies with male CHWs counseling male participants are needed to better understand the influence of CHWs’ sex on outcomes. Fourth, the results from this single site intervention may have limited generalizability to other regions, especially in places where the use of mobile phones and access to a trained CHW are different. Fifth, we did not enroll consecutive households and did not collect information on number of participants screened (but subsequently excluded) for study participation. This may limit the generalizability of our findings. Finally, our study only focused on those who smoke cigarettes and/or bidis, and did not include users of smokeless tobacco products.
CONCLUSIONS
In this cluster randomized trial, we evaluated the effectiveness of a multi-component smoking cessation intervention, involving CHW-led home-based counseling supplemented by mobile text messages. We found that, compared to brief advice alone, a greater number of participants in the intervention arm quit smoking at the end of 12 months. However, the difference was not statistically significant, likely due to inadequate sample size. Further studies are needed to evaluate the use of smoking cessation interventions that combine CHW counseling with multimedia-based messaging solutions such as WhatsApp.